Sports Hernias: Diagnosis & Treatment
Did you know that nearly half of chronic groin pain cases in athletes are caused by a condition that isn’t even a true hernia?
If you’ve ever worked with athletes, you know how frustrating groin pain can be. It lingers, affects performance, and, worst of all, can be notoriously difficult to diagnose. Traditional injuries like muscle strains and hip impingements often come to mind first, but there’s another condition that frequently flies under the radar—sports hernia.
Despite its misleading name, a sports hernia isn’t your typical hernia with a visible bulge. Instead, it’s a persistent soft tissue injury that affects athletes in high-impact sports that require rapid direction changes & sprinting. Due to the lack of clear diagnostic criteria and imaging, many athletes go months—sometimes even years—without an accurate diagnosis, leading to prolonged pain
So, how can physiotherapists better understand and manage this tricky condition?
This article breaks down the key findings from a study by Hopkins and colleagues, providing a deep dive into sports hernia: its mechanisms, risk factors, diagnostic challenges, and the best evidence-based treatment.
If you’re looking for practical tips backed by research to help your patients recover faster and stay in the game, keep reading!
In A Nutshell
Rapid Results:
Sports hernia is a complex condition often involving soft tissue damage without a visible bulge, and it can coexist with other pathologies like femoroacetabular impingement.
Professional Takeaway:
Focus on conservative management with core and hip strengthening exercises before considering surgery, as most cases improve with nonoperative treatment.
Aim Of The Study
To discuss sports hernias and provide guidance on assessment & treatment options in athletes

Did You Know?
Groin pain in athletes is common, but determining the exact cause can be a little tricky
The groin is a complex area, and pain here can come from a variety of sources. While muscle strains and joint irritations are the first thing that spring into mind, a lesser-known but equally frustrating condition is the sports hernia.
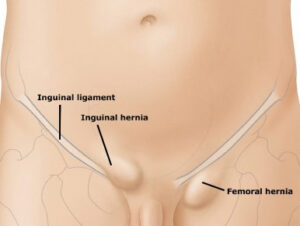
Sports hernia, despite its name, isn’t a like traditional hernia (Inguinal) with a visible bulge.
Instead, it’s a subtle but persistent injury that primarily affects athletes in sports that involve repetitive:
- Twisting
- Sprinting
- Sudden directional changes.
The lack of diagnostic tests means many athletes undergo months of pain and ineffective treatments before receiving a proper diagnosis.
Definitions: A sports hernia refers to soft tissue damage or strain in the groin area, often involving muscles and tendons, without a visible bulge, while an inguinal hernia involves a protrusion of tissue or organs through a weak spot in the abdominal wall, typically creating a noticeable bulge.
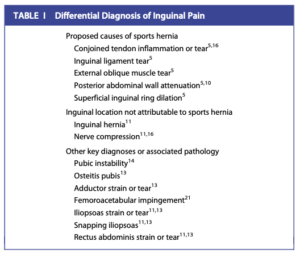
Groin pain in athletes has a broad differential diagnosis, meaning there are multiple potential causes.
Orthopaedic conditions like muscle strains, tendinopathies, and hip joint pathology often come to mind first. However, not all groin pain originates from musculoskeletal issues.
Visceral conditions, such as gastrointestinal or urological problems, can also contribute, requiring evaluation by a general surgeon.
Due to the complexity, it’s easy to see why it’s important to make an accurate diagnosis early.
For example, poor diagnosis could lead to ineffective treatment and prolonged discomfort.
And why are they so complex?
Unlike traditional hernias, they lack a clear anatomical defect, making them difficult to define. Research on sports hernias is limited, particularly within orthopaedic literature, leading to inconsistent diagnostic and treatment approaches.
Because no single test confirms the condition, it’s often diagnosed by excluding other possible causes of groin pain.
How, When & Why?
A sports hernia doesn’t have a clear definition and is sometimes referred to as chronic groin pain syndrome or functional pelvic instability.
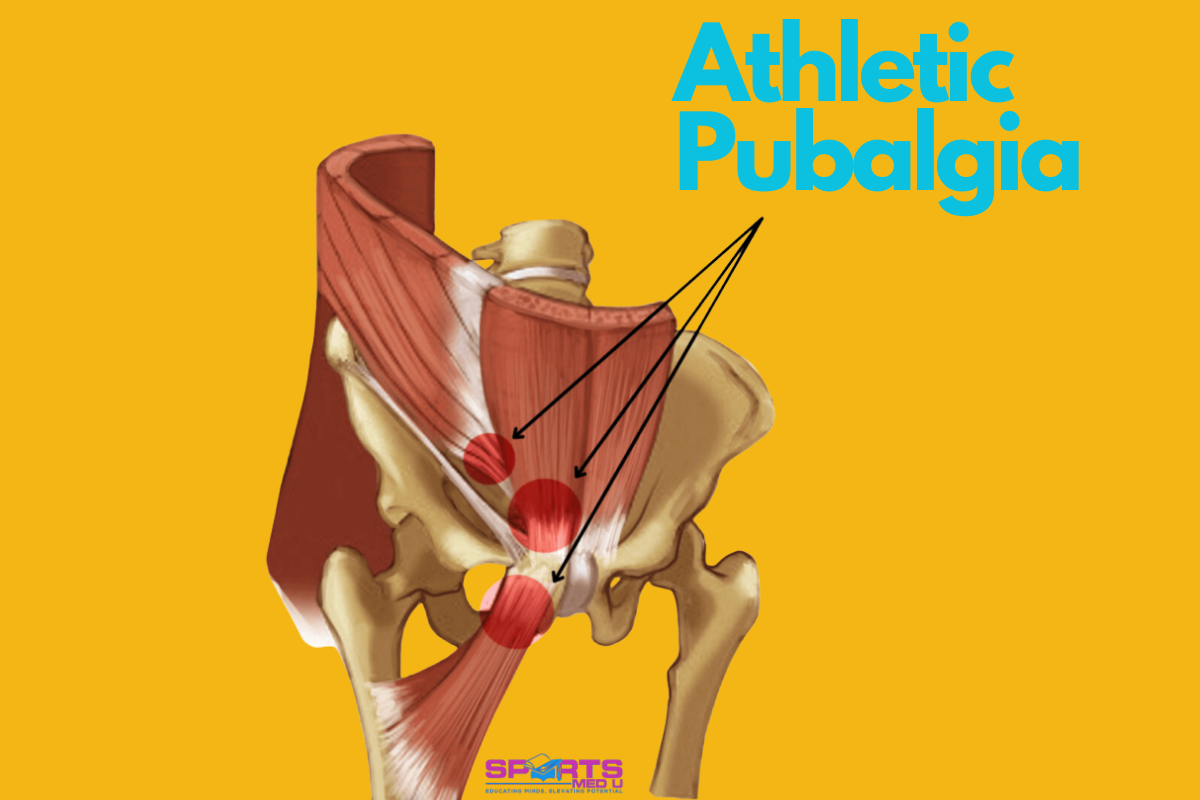
The terminology surrounding it is equally confusing, with terms like sportsman’s hernia, athletic pubalgia, sports pubalgia, Gilmore groin, hockey groin, and incipient hernia being used interchangeably.
Because there are a gazilion names it makes the diagnosis and treatment difficult, especially when working with other clinicians, nutritionists and doctors
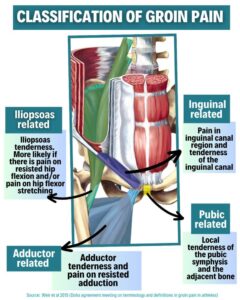
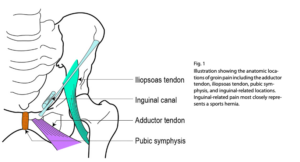
Groin pain is usually classified into different categories, such as:
- Adductor,
- Iliopsoas
- Pubic
- Inguinal-related pathologies.
These, inguinal-related pain is most associated with sports hernia and is often referred to as inguinal disruption, as no true hernia is present.
Facts
- Sports hernia accounts for approximately 50% of chronic groin pain cases in athletes.
- In one study, 95 out of 189 athletes with chronic groin pain were diagnosed with this condition, and surgical findings showed posterior inguinal wall abnormalities in 80% of cases.
- Groin injuries overall represent about 6% of all athletic injuries
- The condition predominantly affects male athletes, with 95% of cases occurring in men, while only 5% are seen in women.
- The median age of affected athletes is between 26 and 28 years, with high-risk sports including football (both European ⚽ and American 🏈), hockey, basketball, cricket, and rugby. The explosive movements & rapid direction changes that are frequent in these sports make athletes particularly susceptible.
How Does it Actually Occur?
As you may now guessed, sports hernia is a complex condition driven by excessive mechanical stress on the groin.
High-intensity movements like sprinting, kicking, and sudden direction changes place immense tension on the inguinal region.
Over time, this stress can lead to small tears or a weakening of the structures, resulting in persistent pain.
Sports hernia does not involve a visible bulge, making it difficult to diagnose
Instead, it’s experienced as long lasting groin pain
Hip Range
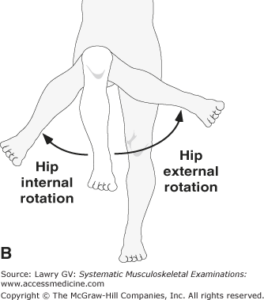
One key factor contributing to sports hernia is reduced hip range of motion. Limitations often correlate with groin pain on the same side.
This restriction places additional stress on the pubic symphysis, the joint at the front of the pelvis, leading to instability.
Additionally, conditions like femoroacetabular impingement, where abnormal hip joint mechanics create excess “friction”, may predispose athletes to inguinal injuries.
Addressing hip mobility is key in both prevention and rehabilitation!
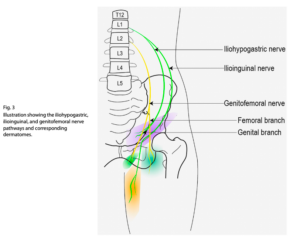
Nerves
Nerve compression and inflammation can also contribute.
The ilioinguinal nerve, which runs through the groin, may become compressed or irritated, contributing to pain.Some treatments, like radiofrequency denervation of the ilioinguinal nerve, have provided temporary relief, but they do not correct the underlying biomechanical dysfunction.
Muscular Imbalances
The adductor and abdominal muscles work together to stabilise the pelvis during movement. Weakness in these muscles can create instability & increasing the risk of soft tissue injuries, especially during high impact drills (or games).
Sports hernia is often viewed as a syndrome involving multiple structures (abdominals, adductors, and inguinal region). Strengthening and balancing these muscle groups is an essential part of rehabilitation.
Structural abnormalities in the inguinal canal
Increased tension in this area can lead to weakening of the posterior abdominal wall, dilation of the superficial inguinal ring, or small tears in the conjoined tendon and surrounding tissues.
Despite these changes, there is no true herniation of abdominal contents, which is why the term “hernia” can be misleading.
Assessing The Hip
Groin pain can be very tricky in sports medicine because it can come about from variety of sources.
For example,
- Musculoskeletal injuries like muscle strains, ligament sprains, and fractures
- Joint and nerve-related conditions such as sacroiliac joint dysfunction and nerve entrapment.
- Hip disorders, including femoroacetabular impingement, osteitis pubis, and intra-articular hip pathology
- Other medical conditions like inguinal hernias, urogenital issues, lumbar disc disease, and pelvic floor dysfunction can present with similar symptoms
One of the biggest challenges in diagnosing groin pain is that multiple conditions can coexist 😬
Studies have shown that about 33% of athletes with groin pain have more than one contributing factor.
For instance,
- Adductor, rectus abdominis, and iliopsoas-related pain frequently overlap
- Osteitis pubis and adductor-related pain are often linked, suggesting they may be part of the same underlying syndrome.
- FAI, a condition affecting the hip joint, is present in 86% of sports hernia patients
What To Be Mindful Off
When it comes to sports hernia specifically, a full assessment is non-negotiable.
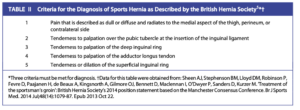
Unlike other conditions, sports hernia does not always show up clearly on imaging, so a detailed patient history and physical examination is the most valuable form of diagnostics
The pain is typically localised around the pubic symphysis and may radiate through the rectus abdominis or adductor tendons.
Athletes frequently report that pain worsens with movements that involve explosive force, such as kicking, sprinting, and sudden acceleration or deceleration.
Symptoms often improve with rest, only to return once activity resumes.
In some cases, the pain may radiate into the thigh or testicles, particularly if nerve involvement is present.
A simple clinical test—asking the patient to cough—can sometimes reproduce the pain (suggests pressure-related discomfort in the inguinal region.)
This symptom can help differentiate sports hernia from other causes of groin pain.
Treating The Hip
The First Step
A structured rehab program is the first-line approach for managing sports hernia, with at least two months of rehabilitation recommended before considering surgery.
Strengthening muscles like the gluteus medius, transversus abdominis, and hip flexors is the go to, alongside core stabilisation while avoiding excessive hip flexion.
Rehab often includes Swiss balls, resistance bands, swimming, and sport-specific drills.
Progression starts with rest and non-weight-bearing exercises, followed by upright functional training.
Resistance and plyometric exercises are added once the athlete can perform a supine crunch pain-free.
Sport-specific movements are reintroduced when rehab milestones are met.
Surgery – When Rehab Fails
If pain persists beyond two to six months, surgery may be necessary.
Laparoscopic repair with mesh and adductor tenotomy allows some athletes to return to play in just 24 days.
Adductor tenotomy alone may be just as effective. Minimally invasive techniques are preferred, as they lead to quicker recovery—5.6 weeks on average compared to 25.8 weeks for open repair. Endoscopic mesh repair also results in lower pain levels than nonoperative treatment.
Among NHL players, most returned to similar performance levels, though older athletes played fewer games post-surgery.
Additional Interventions
Nerve decompression, such as radiofrequency denervation of the ilioinguinal nerve, can provide pain relief for up to six months and may delay or prevent surgery.
Femoroacetabular impingement often coexists with sports hernia, but it is a poor predictor of surgical success.
Many athletes require both hernia repair and hip arthroscopy.
Clinical Tips
- Thorough Assessment: Spend time with the patient to gather a detailed history and perform a full physical exam( ROM, palpation, resisted movements etc). This helps rule out other potential causes of groin pain, such as hip or nerve issues.
- Core and Hip Strengthening: Focus on strengthening muscles like the gluteus medius, transversus abdominis, and hip flexors. These muscles are essential for stabilisation of the pelvis and improving functional movement patterns during movemnts that need pelvic control.
- Progress Activity Gradually: Start with non-weight-bearing exercises and progress to functional upright movements as the patient improves. Gradual increases in resistance, speed, and plyometric exercises should only occur when the patient can perform foundational movements pain-free.
- Referrals: When femoroacetabular impingement or other concurrent pathologies are suspected, refer the patient to an orthopedic specialist. A multidisciplinary approach will ensure all potential causes of groin pain are addressed for the best outcome.
- Tailor Rehab to Sport-Specific Movements: Make rehab exercises as sport-specific as possible to ensure athletes are prepared for the demands of their activity when they start to make a comeback. This includes gradually reintroducing movements like kicking or sprinting while focusing on technique to prevent re-injury.
Reference:
- Hölmich, P., 2007. Long-standing groin pain in sportspeople falls into three primary patterns, a “clinical entity” approach: a prospective study of 207 patients. British journal of sports medicine, 41(4), pp.247-252.
- Hopkins, J.N., Brown, W. and Lee, C.A., 2017. Sports hernia: definition, evaluation, and treatment. JBJS reviews, 5(9), p.e6.
- Lovell, G., 1995. The diagnosis of chronic groin pain in athletes: a review of 189 cases. Australian journal of science and medicine in sport, 27(3), pp.76-79.
- Rossidis, G., Perry, A., Abbas, H., Motamarry, I., Lux, T., Farmer, K., Moser, M., Clugston, J., Caban, A. and Ben-David, K., 2015. Laparoscopic hernia repair with adductor tenotomy for athletic pubalgia: an established procedure for an obscure entity. Surgical endoscopy, 29, pp.381-386.







Leave a Reply