
Is EMS Effective At Developing Knee Strength Post ACL & Meniscus Injury?
Is ACL rehab is an uphill battle? You’re not alone. The journey to regain strength and function after an ACL reconstruction can be long and frustrating—especially when muscle weakness becomes a major roadblock. But what if there was a tool that could speed up recovery and give your patients a better shot at bouncing back?
Enter electrical muscle stimulation (EMS).
EMS has been gaining attention in the physio world—and for good reason. It offers a unique way to activate muscles, even when traditional exercises are too risky or difficult early on in rehab.
But how effective is it really? And when should you use it to get the best results?
A study by Imoto and colleagues looked into these questions, and we’re here to break it all down for you.
This article takes a closer look at the findings from Imoto’s systematic review, discussing factors such as when and how EMS works best after ACL reconstruction.
Keep reading to learn about the practical tips that help integrating EMS into your treatment plans.
In A Nutshell
Main Takeaway:
The evidence from randomised clinical trials, though of limited quality, clearly show that EMS, when combined with a rehab program, is more effective in improving muscle strength and function for up to two months after ACL reconstruction compared to just rehab
Clinical Tip:
Aim to use EMS the first six weeks after surgery. The ideal low frequency for boosting muscle strength is between 35 to 80 Hz. For medium frequency, use a modulation of 2500 Hz/50-75 Hz. Aim for a pulse duration of 200 to 350 microseconds, and during the early rehabilitation phase, maintain a contraction-to-rest ratio of about 1:5 for the most effective results
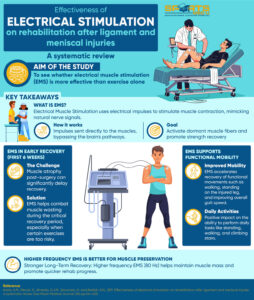
Aim Of The Study
To assess the effectiveness of electrical stimulation for rehabilitation after soft tissue injuries of the knee (anterior cruciate, posterior cruciate, lateral and medial ligament and meniscal injuries), treated surgically or conservatively
Did You Know?
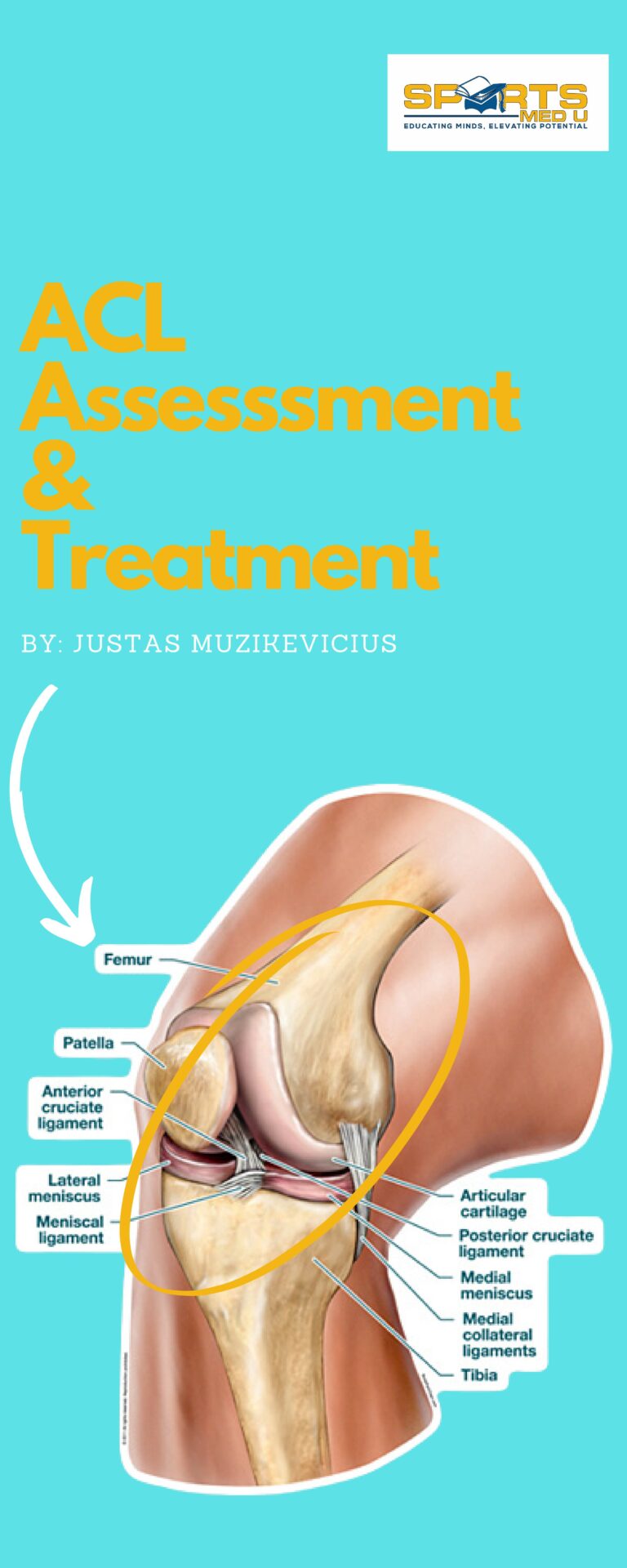
Knee injuries are common, annoying and no joke when it comes to rehab and treatment, especially if we throw ligament and meniscal disruption into the mix.
Among people aged 10 to 29 years, these injuries are alarmingly common, with men making up 57% of cases. When we look closer, we see that soft tissue injuries of the knee—primarily involving the ligaments or menisci—are the most frequent contributors.
The anterior cruciate ligament (ACL) tops the list as the most frequently damaged ligament, while the medial meniscus is the most common among meniscal injuries.
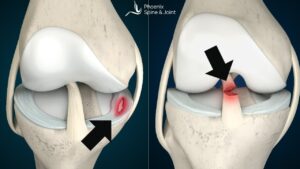
How Do These Injuries Happen?
Most ligamentous/meniscal knee injuries occur during a twist while the joint is bearing weight.
For example,
- Landing awkwardly from a jump
- Pivoting sharply during a game
- Slipping on an uneven surface
The severity of the injury depends on the degree of force and excess movement exerted on the joint. Sometimes, the damage can range from mild strains to complete tears, with the latter often requiring surgical intervention.
Challenges With Rehab
One of the most significant challenges after a ligament or meniscus injury is controlling muscle weakness. Post-surgery or during immobilisation, the quadriceps are affected the most (especially if the graft used for ACL repair is the quad or patella).
And it’s not just a question of stiffness or soreness.
Studies show that five to six weeks of immobilisation can lead to major changes in the quadriceps’ muscle fibers, particularly type 1 fibers responsible for endurance. In fact, quadriceps strength can drop by as much as 60–80% during this period. This dramatic muscle wasting is why rebuilding strength becomes a primary focus of rehab.
In the early stages, protecting the healing ligament is equally important. Isolated knee extensor exercises can put undue strain on the repaired ligament.
This is where electrical muscle stimulation (EMS) steps in.
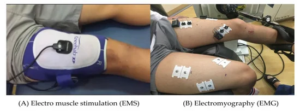
First and foremost, what is EMS?
EMS is a technique that uses electrical impulses to cause muscles to contract, mimicking the natural signals sent by the nervous system.
Why EMS?
It can be especially helpful when exercises are too risky or challenging. Studies have shown that EMS significantly increases quadriceps strength and torque (the muscle’s ability to produce rotational force) in people recovering from ACL reconstruction or other ligament surgeries.
EMS works by bypassing the brain’s normal activation pathways and directly stimulating the muscle fibers. This means it can activate more muscle fibers, including those that might be dormant due to injury or disuse.
Methods Of Study
A search was done across multiple databases (e.g., Cochrane, PubMed, Embase, CINAHL, PEDro, and Lilacs) for randomised controlled trials on electrical stimulation and knee injuries up to December 2010, with no language restrictions.
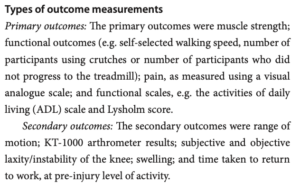
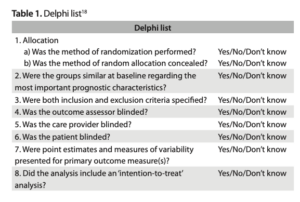
Results
A total of 19 studies included after removing duplicates
Comparison 1: Conventional Rehab With & Without EMS
Strength Gains in Isometric Muscle Contractions
Studies showed mixed outcomes for the effects of EMS on isometric quadriceps peak torque.
Lieber et al. found no significant differences between groups at four weeks post-surgery, but by six to nine weeks, EMS showed benefits in reducing torque loss during immobilisation.
At six weeks, studies reported statistically significant improvements in torque for the EMS group.
Conversely, Sisk et al. found no significant differences in torque at various intervals between seven and nine weeks.
Over the longer term, results were inconsistent, with no significant differences observed at 12 weeks or one year after surgery in studies by Lieber and Paternostro-Sluga.
Strength Gains in Moving Muscle Contractions
Significant improvements in isokinetic torque were observed with EMS at faster test velocities of 90°/s and 210°/s within six to eight weeks post-surgery, as reported by Paternostro-Sluga and Buhmann et al.
However, at slower velocities (60°/s), no notable benefits were found. Long-term evaluations (12 weeks to one year) showed no significant differences between EMS and control groups, except for a marked improvement favouring EMS at 18 weeks as observed by Anderson and Lipscomb.
Overall Quadriceps Strength Recovery
The isometric quadriceps index also showed early benefits from EMS.
Two studies found statistically significant improvements at six weeks post-surgery, with Snyder-Mackler et al. highlighting 70% recovery in quadriceps strength using high-intensity ES compared to 57% with voluntary exercise.
However, by 12 and 16 weeks, no significant differences were observed between groups.
Recovery of Muscle Strength During Movement
At eight weeks, Snyder-Mackler et al. noted substantial gains in the isokinetic quadriceps index at higher test velocities (90°/s and 210°/s) for the ES group. These findings show the potential of ES to improve recovery speed and strength, particularly during the early to mid-stages of rehab.

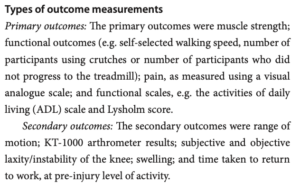
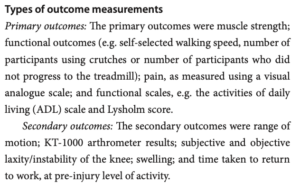
Functional Tasks
Daily Activities and Mobility
Fitzgerald et al. reported significant improvements in functional outcomes with EMS.
At 12 and 16 weeks post-surgery, the ES group scored better on the ADL questionnaire, indicating improved ability to perform daily activities. However, no significant differences were found in the number of participants using crutches or progressing to treadmill running.
Pain and Stability
There were no significant differences between ES and control groups in knee pain (as assessed by Fitzgerald et al.) or in ligament stability measured using the KT-1000 device (Buhmann et al.).
Gait and Movement Efficiency
Gait analysis favoured the EMS group, with improvements in gait velocity, standing time on the affected side, and cadence noted by Snyder-Mackler et al. However, other functional tests, such as the Fastex test and unilateral squat, showed no significant differences between groups.
Range of Motion and Strength
Anderson and Lipscomb observed greater knee range of motion in the EMS group at 18 weeks. EMS also contributed to improved manual muscle test performance compared to the control group. Additionally, Siebert et al. found less quadriceps muscle loss in the ES group at six weeks post-surgery.
Long-Term Functional Scores
Staub et al. found no significant differences between ES and control groups in Lysholm or Tegner (standardised questionnaires used to assess knee function and activity level) scores at 12 weeks and nine months. Similarly, tests like the lateral step and forward reach did not show meaningful benefits from EMS in the short term.
These findings suggest EMS is beneficial for certain aspects of recovery, particularly in gait and muscle preservation, while showing limited effects on long-term functional scores or pain relief.
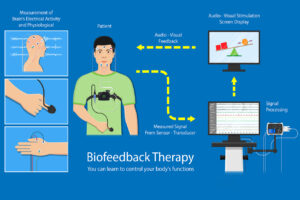
Comparison 2: Conventional rehab with EMS VS conventional rehab with biofeedback
Biofeedback = a technique that teaches people to control physiological processes, such as muscle tension or heart rate, by providing real-time feedback, helping improve physical function and reduce pain
Draper and Ballard found that biofeedback showed a significant advantage for improving the isometric quadriceps index compared to other methods.
However, Rebai et al. showed no significant difference between ES at 20 Hz and 80 Hz for isometric quadriceps peak torque, although higher frequency stimulation appeared to reduce the volume deficit more effectively.
Range of Motion
There were no notable differences in range of motion between groups at one, two, or four weeks post-surgery, as reported by Draper and Ballard.
Comparison 3: Conventional rehab with EMS of 20 Hz versus conventional rehab with EMS of 80 Hz
Rebai et al. observed that thigh muscle volume deficits were smaller in the group using 80 Hz EMS compared to 20 Hz ES.
This suggests that higher frequency stimulation for preserving muscle mass during rehabilitation is more advantageous.
So, Is EMS Effective?
EMS has been shown to be a great tool for post op treatment , particularly for patients recovering from ACL reconstruction or meniscectomy.
Studies show that EMS, especially when combined with exercise, significantly improve muscle strength six weeks post-surgery, likely due to its ability to preferentially activate type II fast-twitch muscle fibers alongside type I endurance fibers.
This gives a dual benefit traditional rehab often misses.
The additional stimulation is particularly impactful during the early rehab phase, when muscles are weakest.
Beyond strength, EMS supports functional recovery, improving walking speed, standing time on the injured leg, and performance in daily activities, aligning with the ultimate goal of regaining independence.
However, inconsistent strength assessment protocols and variations in EMS parameters across studies makes it hard to standardise protocols
The findings from this systematic review support previous research, which demonstrates that combining EMS with exercise is more effective than using exercise alone

Clinical Tips
- Use EMS Early in Rehab: EMS can be most effective in the first six weeks following ACL reconstruction or meniscectomy. During this period, the quadriceps are prone to significant muscle weakness, and EMS helps bypass this issue by directly stimulating muscle fibers. This early stimulation can help preserve muscle strength and prevent significant atrophy while protecting the healing tissues.
- EMS Frequency: Based on the studies, for muscle strength, it’s recommended to use low-frequency stimulation ranging from 35 to 80 Hz, with medium-frequency modulation at 2500 Hz/50-75 Hz.
- Combine EMS with Exercise: Evidence shows that EMS, when combined with traditional rehabilitation exercises, is more effective than exercise alone. The combination maximises muscle activation and strength recovery. EMS provides an extra boost, especially when the muscle is too weak to perform normal exercises or when the exercise load is too risky for the healing tissues.
- Functional Recovery: While muscle strength is essential, functional recovery should not be overlooked. EMS has shown improvements in gait, walking velocity, and time spent standing on the injured leg, which are pretty much the main goals in early rehab.
References:
- Anderson, A.F. and Lipscomb, A.B., 1989. Analysis of rehabilitation techniques after anterior cruciate reconstruction. The American Journal of Sports Medicine, 17(2), pp.154-160.
- Draper, V. and Ballard, L., 1991. Electrical stimulation versus electromyographic biofeedback in the recovery of quadriceps femoris muscle function following anterior cruciate ligament surgery. Physical Therapy, 71(6), pp.455-461.
- Fitzgerald, G.K., Piva, S.R. and Irrgang, J.J., 2003. A modified neuromuscular electrical stimulation protocol for quadriceps strength training following anterior cruciate ligament reconstruction. Journal of Orthopaedic & Sports Physical Therapy, 33(9), pp.492-501.
- Imoto, A.M., Peccin, S., Almeida, G.J.M., Saconato, H. and Atallah, Á.N., 2011. Effectiveness of electrical stimulation on rehabilitation after ligament and meniscal injuries: a systematic review. Sao Paulo Medical Journal, 129, pp.414-423.
- Lepley, L.K., Davi, S.M., Burland, J.P. and Lepley, A.S., 2020. Muscle atrophy after ACL injury: implications for clinical practice. Sports Health, 12(6), pp.579-586.
- Lieber, R.L., Silva, P.D. and Daniel, D.M., 1996. Equal effectiveness of electrical and volitional strength training for quadriceps femoris muscles after anterior cruciate ligament surgery. Journal of orthopaedic research, 14(1), pp.131-138.
- Paternostro-Sluga, T., Fialka, C., Alacamliogliu, Y., Saradeth, T. and Fialka-Moser, V., 1999. Neuromuscular electrical stimulation after anterior cruciate ligament surgery. Clinical Orthopaedics and Related Research®, 368, pp.166-175.
- Rebai, H., Barra, V., Laborde, A., Bonny, J.M., Poumarat, G. and Coudert, J., 2002. Effects of two electrical stimulation frequencies in thigh muscle after knee surgery. International journal of sports medicine, 23(08), pp.604-609.
- Robinson, A.J., 2008. Clinical electrophysiology: electrotherapy and electrophysiologic testing. Lippincott Williams & Wilkins.
- Sisk, T.D., Stralka, S.W., Deering, M.B. and Griffin, J.W., 1987. Effect of electrical stimulation on quadriceps strength after reconstructive surgery of the anterior cruciate ligament. The American Journal of Sports Medicine, 15(3), pp.215-220.
- Staub, A., Ullmann, P. and Winker, K.H., 2002. Die Elektromyostimulation bei frühfunktioneller Rehabilitation nach vorderer Kreuzbandersatzplastik. Aktuelle Traumatologie, 32(02), pp.65-72.




Leave a Reply