Calf Strains: Everything There Is To Know
Let’s talk about a common yet often underestimated injury: calf strain.
Whether the person is an athlete or someone who enjoys casual exercise, calf strains can sneak up on anyone, causing sharp pain in the back of the leg that limits mobility.
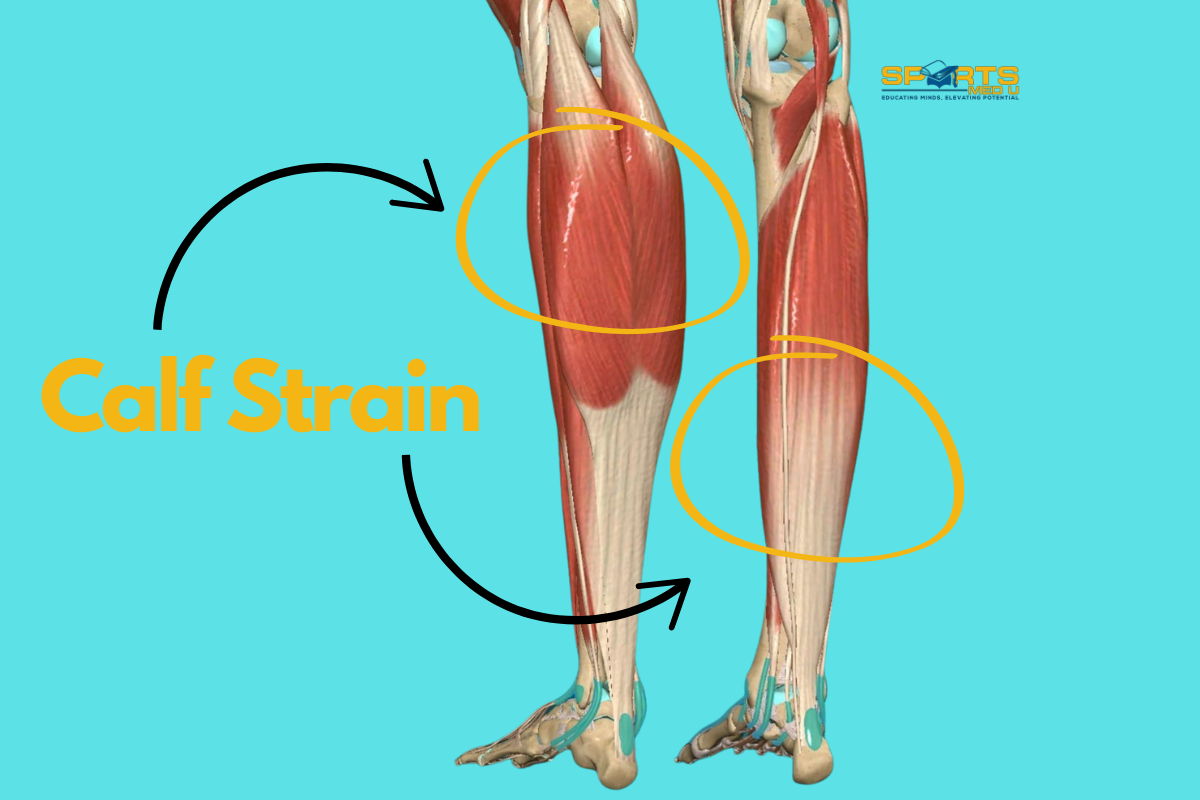
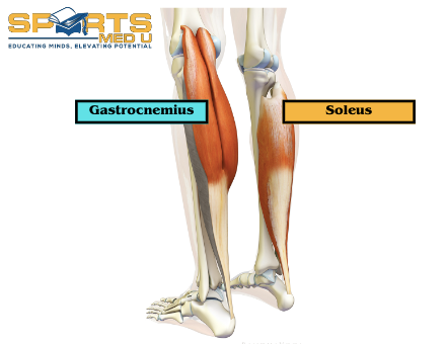
This injury typically affects either the gastrocnemius or soleus muscles in the calf, and knowing which muscle is involved is a key process in the assessment since it can significantly influence the treatment plan.
Having a solid understanding of calf strains—what causes them, the relevant anatomy, and the risk factors—is fundamental. Not only will this article help you support your patients’ recovery, but it will also expand your clinical skills.
In this article, we’ll discuss everything you need to know about calf strains, from causes and symptoms to effective rehabilitation and healing timelines.
By the end, you’ll have a clear, evidence-based understanding of how to approach calf strains, manage recovery, and help patients get back to their activities safely and efficiently.
Let’s get started!
What is a Calf Strain?
It’s considered to be pain at the posterior aspect (back) of the mid leg due to sudden increase in activity, impact or overuse. The strain can be either to the gastrocnemius muscle (higher up the leg) or the soleus muscle (just above the heel)

Did You Happen to Know?
- A calf strain typically affects either the gastrocnemius or soleus muscles (or rarely both), which together make up the calf. The gastrocnemius, a larger muscle, is more commonly injured as its responsible for powerful movements, while the soleus, a deeper muscle, is often strained during prolonged or repetitive running
- Calf Muscle Load During Movement:
- Walking: 1.2–1.5 times body weight.
- Running: The load increases to about 3 – 4 times body weight.
- Sprinting: The load can reach 5–6 times body weight, due to the explosive force required.
- Calf injury is most prevalent among athletes 22 to 28 years of age, more frequently affects men
- It presents as a recurrent injury in approximately 19% to 31% of cases.
Anatomy of The Leg
In overview, the gastrocnemius and soleus muscles originate from the posterior aspect of the leg and insert into the achilles tendon. They work together to plantarflex the foot and provide power and stability during activities such as walking, running, and jumping.
Gastrocnemius
Origin:
It’s a large, two-headed muscle. The medial head originates from the posterior surface of the femoral condyle, which is the rounded end of the femur bone in the thigh. The lateral head originates from the lateral condyle of the femur
Insertion:
The two heads of the gastrocnemius muscle merge into a single belly that inserts into the calcaneus bone via the Achilles tendon. This insertion point is located on the heel bone (calcaneus) and is known as the calcaneal tuberosity
Function:
The main function of the gastrocnemius muscle is to plantarflex the foot as well as assisting to flex the knee. When standing on tiptoes or push off the ground while walking or running, the gastrocnemius muscle contracts, causing the ankle joint to extend and the heel to rise.
Get the ACL assessment & rehab guide with over 50+ exercises to help you structure your rehab programme
I’ve spent over 1,000 hours studying sports medicine to give you the best tips and tools to succeed with your patients
Now, I’ve put everything I know about ACL’s into a simple guide… for free.
Soleus
Origin:
The soleus muscle originates from the head and shaft of the fibula bone, as well as the posterior surface of the tibia bone.
Insertion:
The muscle fibres then merge into a single belly that inserts into the calcaneus bone via the Achilles tendon, at the same point as the gastrocnemius muscle.
Function:
The main function of the soleus muscle is to plantarflex the foot, just like the gastrocnemius muscle. However, unlike the gastrocnemius, the soleus muscle is not involved in flexing the knee joint as it does not cross it. It’s primarily responsible for maintaining posture, especially when standing or walking slowly. It is also involved in helping to stabilise the ankle joint during weight-bearing.
Mechanism of injury
Gastrocnemius:
Classic mechanism of a gastrocnemius tear involves knee extension with sudden ballistic foot movement from dorsiflexion to plantar flexion. During sudden increase in tension the muscle gets maximally stretched, leading to an abrupt strain/rupture, most commonly in the medial head.
The medial head is more vulnerable to injury than the lateral head due to its longer and narrower shape and smaller cross-sectional area.
Soleus:
Soleus muscle strain is an overuse condition that can occur because of repetitive, passive dorsiflexion of the foot with the knee bent. This can lead to strain or tearing of the muscle fibres and is commonly observed in athletes who do activities that require repetitive uphill and/or long-distance running. Runners, in particular, may be more susceptible to developing soleus muscle strain due to the repetitive nature of the sport.
In terms of hills, the angle of incline can increase the strain on the soleus muscle as it works to maintain stability and control during each stride. This can result in fatigue, weakness, and eventual strain or tearing of the muscle fibres.

Frequency/Pattern of injury
The exact epidemiology of calf strains is not well-defined, but studies have shown that calf strains are more common in sports that involve sprinting, such as football, basketball, and track and field as well as sports that induce muscle fatigue over time like long distance running.
Calf strains can occur in athletes of all ages and genders, but they are more common in older athletes, possibly due to decreased muscle flexibility and strength with age
Symptoms & Clinical Presentation
Symptoms and clinical presentation will characteristically differ dependent on what muscles of the calf is affected.
Here are key things to understand when diagnosing calf strains.
- Gastrocnemius strain is associated with high intensity running, acceleration, and deceleration – Gastro is dense in fast-twitch muscle fibres adapted for rapid contraction (Type 2 A and B)
- Acute strain of the gastrocnemius can present with an audible pop.
- This then is followed by dull to severe pain and swelling in the posterior lower limb within 24 hours
- The pain can be latent at the time of the injury, coming out only after the person tries to stand, walk, or plantar flex the foot.
- Soleus strain is more likely to occur during steady-state running. Soleus is dense in slow-twitch muscle fibres adapted for postural control (Type 1)
- The person may complain of muscle tension and tightness
- Pain may gradually development over the course of days to week
- Swelling is minimal and overall calf functional ability is affected mildly
Clinical Course For Calf Strains
The clinical course of calf strain can vary depending on the severity of the injury. In general, mild strains may take several days to a week to resolve, while more severe strains may take several weeks or even months to fully heal.
Muscle healing time frames:

The Role of Imaging
Imaging for calf muscle strains is not often used in a clinical setting as it can be diagnosed with subjective and objective testing alone. However, in cases where the diagnosis is uncertain or there is suspicion of a more severe injury imaging can be a very helpful tool to guide diagnosis and treatment.
The frequency of use may vary depending on the provider’s experience and training, the availability of imaging facilities, and the specific clinical scenario.
For example, in a primary care setting, imaging may not be routinely ordered for a mild to moderate calf muscle strain. In a sports medicine or orthopaedic setting on the other hand, imaging will be used more frequently to help guide treatment and assess the extent of the injury.
Ultimately, the decision to use imaging for calf strains will depend on the clinicians judgment and the specific circumstances of the patient’s injury.
- Ultrasoundis often the preferred imaging modality as it is non-invasive, readily available, and cost-effective. It can help identify muscle tears, fluid accumulation, and tissue damage. It can also be used to guide therapeutic injections.
- MRIis a more advanced imaging technique that can provide a detailed view of the soft tissues, such as muscles, tendons, and ligaments. It can help identify the exact location and extent of the injury and is particularly useful in cases of severe or complicated calf muscle strains. It also helps to detect intramuscular fluid collection, which is associated with delayed return to play
Is Surgery Necessary?
Surgery is not typically used to treat isolated calf muscle disruption, as most strains can be managed conservatively, along with appropriate rehabilitation. However, in cases where the muscle strain is severe or complicated by other injuries, surgery may be necessary.
For example, if a calf muscle strain is associated with a complete tear of the Achilles tendon or a fracture of the tibia bone, surgery will most likely be required to repair the damage and restore normal function.
In general, surgical intervention for a calf strain is rare and reserved for cases where non-surgical management has failed or is not appropriate
Get the ACL assessment & rehab guide with over 50+ exercises to help you structure your rehab programme
I’ve spent over 1,000 hours studying sports medicine to give you the best tips and tools to succeed with your patients
Now, I’ve put everything I know about ACL’s into a simple guide… for free.
Risk Factors For Sustaining a Calf Strain
The risk factors for a calf muscle strain are mostly generic to all muscle injuries.
Two key areas to be mindful of:
- Age
- A possible explanation is that age-related tissue changes involve progressive declines in skeletal muscle quality and function.
- The consequences of which include neuromuscular maladaptation’s that restrict muscle force and rate of contraction.
- History of calf strain or other lower limb injuries
- Prior injuries in the calf, hamstrings, quadriceps, adductors, and knee have been identified as risk factors for a subsequent calf injury due to over compensation of other muscles
Assessing The Calf
After the subjective assessment where you determine the when and the how.
The next step is to perform an objective assessment.
- Palpation is often the first step in assessing a calf strain as it helps to identify any tender spots, which can be an indicator of muscle damage. It’s important to note that tenderness in the medial gastrocnemius belly can be normal and is common even in uninjured people. Look for a sharp discomfort with possible bumps or ridges in the muscle. The most important step in assessing the calf is to distinguish which muscle is affected, as the treatment protocols are different. Tenderness in the medial gastrocnemius belly or the musculotendinous junction indicates gastrocnemius strain, whereas tenderness distal and lateral to the gastrocnemius implicates the soleus (closer to the heel)
- Active range of motion of the ankle and knee are used to determine the extent of the injury and whether the person is able to actively move its joints without restrictions (guarding due to pain & swelling) compared to un-affected leg. It helps to understand the strength, flexibility, and coordination of the muscles and the nervous system that control joint movement.
- Passive range of motion assesses the integrity of the joint capsule, ligaments, tendons, and other structures surrounding the joint. Passive range testing can also help identify any restrictions or limitations in joint movement due to injury, inflammation, or other conditions
Note.
In general, active range testing is used to assess the functional ability of a person to move their joint in daily activities, while passive range testing is used to assess the structural integrity of the joint and detect any abnormal or restricted movements.
- Strength testing can be used to evaluate the extent of muscle disruption and to determine the ability of the muscle to generate force. This is important in determining the appropriate treatment and rehabilitation plan for the patient. At this stage, maximal contractions are not recommended as it can cause further calf injury. Instead, ask the person to do a single leg calf raise (standing for gastrocnemius or seated for soleus) to understand their functional capability. Note pain levels, success or failure and height of heel raise to gauge progression.
If a patient has a severe calf strain, they may require a longer period of rest and rehabilitation before returning to their normal activities.

How To Manage Calf Strains Early?
Acute — In the acute phase, treatment is designed to protect the injured tissue by reducing activity, managing pain, and preventing haemorrhage or other complications.
- In the first 24 to 72 hours, activities should be limited to allow the injured leg to be rested in an elevated position and NSAID use should be carefully managed (if any) due to their ability to impede the inflammatory processes. These processes are essential for optimal healing and recovery
- High compression bandages that exert 20 to 30 mm Hg of pressure have been recommended in published reports, and some evidence has suggested that compression bandage use can improve recovery by up to 7 days
- Massage & heat are contraindicationsdue to increased risk of haemorrhage
Sub-acute — In the subacute phase, the body repairs the soft-tissue damage and forms scar tissue.
- The goal of treatment is to improve mobility, prevent muscle atrophy or contracture, and facilitate tissue regeneration in order to optimise functional recovery
- Rehabilitation includes passive and active stretches, soft-tissue techniques, muscle strengthening, and proprioception exercises for 2 weeks.
- Stretching elongates the intramuscular scar tissue in preparation for strengthening exercises (dependent on pain & severity of strain).
- As range of motion improves and pain subsides, strength training can progressively incorporate isometric, isotonic, and dynamic exercises as tolerated without pain.
Exercise Based Management
Exercise can promote the release of growth factors and cytokines, which can aid in tissue repair and regeneration. Activity also increases blood flow to the affected area, delivering oxygen and essential nutrients to the muscles to help stimulate the healing process.
Specific exercises can help to restore muscle strength, range of motion, and flexibility. It can also prevent the development of scar tissue and muscle imbalances, which can lead to long-term complications.
Implementing a structured rehab program based on the principles of progressive overload, specificity, and individualisation, helps ensure that recovery is both safe and effective, allowing patients to gradually rebuild functional ability while minimising the risk of re-injury.
Here are a few exercises to try: (Reps and sets should be based on the persons functional ability – the numbers below are volumes to aim for)
- Double leg STANDING (Gastro) heel raises (3 sets / 25 reps)
- Double leg STANDING KNEE BENT (Soleus) heel raises (3 sets / 25 reps)
- Horizontal & lateral heel raises to mimic running and sprinting (3 sets / 15 reps)
- Single leg Romania dead lifts —> Knee drive Romania dead lifts (3 sets / 30-60 sec)
- Body weight/loaded squats (3 sets/ 8-12 reps)
Other Treatment Options
Whilst exercise based management is the gold standard for muscle strains there are a few options out there that can be beneficial in a clinical and elite sport setting.
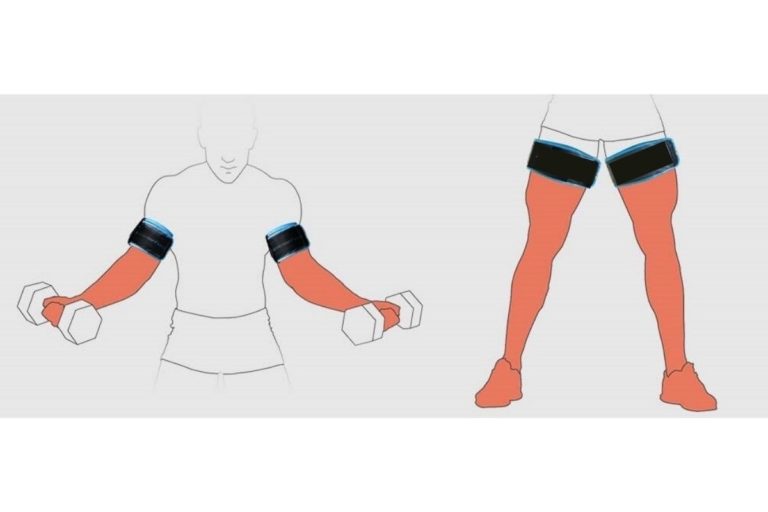
Blood flow restriction training (BFRT):
Is a form of light resistance training that involves using a restriction band proximally on the extremity to occlude venous blood outflow while maintaining arterial blood inflow.
- Light resistance training applies mechanical stress to the muscles, and the use of a restriction band induces tissue hypoxia, which stimulates anaerobic metabolism
- Studies have shown that BFRT can increase muscle strength, hypertrophy, and angiogenesis compared to unrestricted light resistance training. However, less muscle is recruited compared to unrestricted heavy resistance training.
- The biological mechanism underlying BFRT is not yet fully understood. However, the combination of mechanical and metabolic stress is thought to activate cellular signalling pathways that lead to protein synthesis, fast-twitch muscle fibre recruitment, and stimulation of myogenic stem cells.
- BFRT may be useful as a progressive rehabilitation method to promote the regeneration and healing of muscle, especially in situations where heavy resistance training is contraindicated in the early stages of recovery.
Deep water running
Is a form of rehabilitation that involves running in a pool where the feet do not touch the bottom. The individual wears a flotation device to keep them buoyant and can perform running movements without any impact on the lower limbs. This type of exercise is often used in lower limb rehabilitation as it allows athletes to engage in weight-bearing exercise without putting stress on their joints or muscles.
Lower body positive pressure (LBPP):
Is a therapy similar to deep water running but instead of water it involves creating a pressurised environment around the legs while the athlete is walking or exercising. This is typically achieved by placing the athlete in a specialised chamber that is sealed around the waist, and the chamber is then pressurised with air.
Same as deep water running, LBPP therapy reduces the weight-bearing load on the legs, allowing people to do activities with less impact on their joints and muscles.
Return to Running Protocol for Calf Strains
A return to play strategy is very important for people recovering from muscle strains, especially when the strain involves the calf.
The strategy is essential to ensure that the athlete can safely return to their sport without further injury or re-injury. It also helps to gradually reintroduce the person to activity, allowing them to regain strength, endurance and neuromuscular control while minimising the risk of setbacks.
Here are a few calf strain specific test to do before starting to run:
- Standing single leg heel raise 25-30 reps full range of motion | NO PAIN
- Single leg hopping in place 12-20 reps | NOPAIN
When designing a programm here is 6 recommendations:
- Running should be done on alternative days to start
- Avoid prescribing prolonged, slow continuous running – especially if soleus strain
- Do not progress volume & intensity on consecutive days – give the tissues time to adjust & recover
- Run before calf exercises (if doing it on the same day)
- Running should meet the demands of your sport – Don’t run more than you need to.
- Avoid sudden changes of surface/footwear
Get the ACL assessment & rehab guide with over 50+ exercises to help you structure your rehab programme
I’ve spent over 1,000 hours studying sports medicine to give you the best tips and tools to succeed with your patients
Now, I’ve put everything I know about ACL’s into a simple guide… for free.
NICE Guidelines
Guidelines are from NICE and this is a summarised version for your convenience. Visit for a more robust information. These guidelines are for muscle, tendon & ligament sprains and strain, and not calf strain specifically.
Management of suspected sprain or strain in primary care:
Referral to an emergency department if any of the following are present or suspected:
- Fracture or dislocation
- Damage to nerves or circulation
- Wound penetrating the joint or known bleeding disorder
- Serious complication such as hemarthrosis or septic arthritis
- Full tendon rupture
- Complete tear or tear of more than half the muscle belly
- Large intramuscular haematoma
Advise on the use of analgesia for symptom relief including cautions and contraindications.
Advise on initial ‘PRICE’ self-management strategies for the first 48-72 hours after injury. Protection
Rest
Ice
Compression
Elevation
- Advise on safe return to usual activities and sports and sources of information and support.
- Consider arranging medical review after 5-7 days if there is lack of expected improvement or worsening symptoms.
- Consider arranging a routine referral to physiotherapy if the person has ongoing symptoms.
Advise on preventing re-injury:
- Develop a balanced fitness programme that incorporates cardiovascular exercise, strength training, and flexibility
- Avoid prescribing exercises or playing sport when the person is tired or in pain.
- Schedule regular days off from exercise
- Manage any factors that increase the risk of re-injury or falls, where possible
Other Conditions You Should Be Aware Off
When diagnosing a calf strain, clinicians should also be aware of other conditions that can cause similar symptoms, such as:
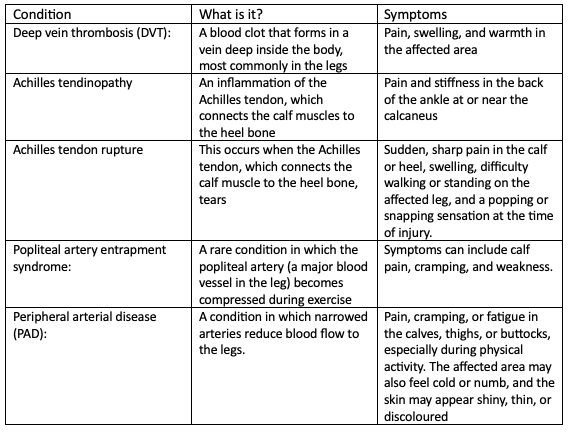
Compared to a calf muscle strain, these conditions may have different signs and symptoms, and may require different diagnostic tests to confirm the diagnosis. For example, DVT may be diagnosed with an ultrasound, while Achilles tendon rupture may require a physical examination or imaging test such as an MRI.
Source
- Baoge, L., Van Den Steen, E.L.K.E., Rimbaut, S., Philips, N., Witvrouw, E., Almqvist, K.F., Vanderstraeten, G. and Vanden Bossche, L.C., 2012. Treatment of skeletal muscle injury: a review. International Scholarly Research Notices, 2012.
- Green, B. and Pizzari, T., 2017. Calf muscle strain injuries in sport: a systematic review of risk factors for injury. British journal of sports medicine, 51(16), pp.1189-1194.
- Green, B., McClelland, J.A., Semciw, A.I., Schache, A.G., McCall, A. and Pizzari, T., 2022. The Assessment, Management and Prevention of Calf Muscle Strain Injuries: A Qualitative Study of the Practices and Perspectives of 20 Expert Sports Clinicians. Sports medicine-open, 8(1), pp.1-28.
- Meek, W.M., Kucharik, M.P., Eberlin, C.T., Naessig, S.A., Rudisill, S.S. and Martin, S.D., 2022. Calf Strain in Athletes. JBJS reviews, 10(3), p.e21
- Pierpoint, L.A., Williams, C.M., Fields, S.K. and Comstock, R.D., 2016. Epidemiology of injuries in United States high school track and field: 2008-2009 through 2013-2014. The American journal of sports medicine, 44(6), pp.1463-1468.

Justas Muzikevicius
Justas is an experienced physiotherapist, author and founder of Sports MedU. From his experience as a professional athlete and now as a sports medicine expert he spends his time researching, writing and teaching clinicians how to put research into practice.
He enjoys basketball, reading and delicious food!