
Blood flow restriction – How to use it for rehab?
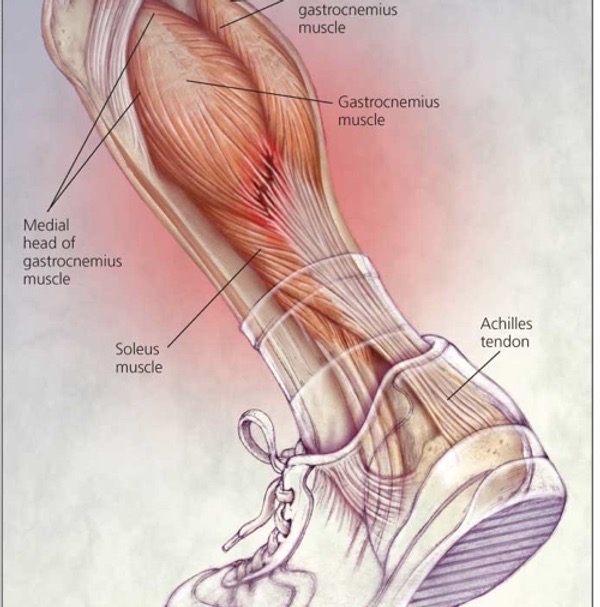
Muscle atrophy is a common occurrence after injury injuries, such as fractures and ligament damage, where extended periods of immobilisation are necessary. This loss of muscle mass poses a significant risk factor for osteoarthritis, a prevalent musculoskeletal disease affecting approximately 250 million adults globally. Strikingly, higher quadriceps strength has been linked to a reduced risk of symptomatic knee osteoarthritis and improvements in physical function.
In this article we look at a systematic review and meta-analysis done in 2017 by Hughes et al ,examining 20 studies to understand the impact of blood flow restriction (BFR) training in rehabilitation. This exploration focuses on how BFR training can combat muscle atrophy and facilitate recovery based on a thorough analysis of the available evidence.
How does BFR work?
Recent studies highlight the efficacy of combining low-load resistance training with BFR for significant muscle growth and strength gains, even with loads as low as 30%. Mechanistically, BFR creates an ischemic and hypoxic muscular environment during exercise, leading to high metabolic stress and mechanical tension.
Proposed mechanisms include:
- Increased systemic hormone production
- Cell swelling
- Production of reactive oxygen species
- Intramuscular anabolic/anticatabolic signaling
- Enhanced recruitment of fast-twitch muscle fibers.
Traditionally, muscle hypertrophy and strength gains were thought to require heavy exercise loads, typically around 70% of an individual’s one-repetition maximum. However, recent research challenges this notion, revealing that low-load training to failure can induce comparable muscle hypertrophy to heavy-load training after 6 to 8 weeks of 3 sessions per week. From a clinical perspective, this is particularly promising, as training to muscular failure with low loads becomes a viable option, especially when heavy loads are impractical.
From a rehab prospective, lower limb BFR training appears to be a clinically relevant tool, helping to avoid the high joint forces associated with heavy-load exercises. This approach offers a promising avenue for enhancing muscle function and promoting recovery faster & safer.
Sign up to our free newsletter and get fun infographics & analysed sports medicine research
The Impact of Blood Flow Restriction Training in Rehabilitation
When we comparing BFR to just low-load training by itself, it seems to elevate strength gains, although not quite as much as the gains seen in traditional heavy-load training. Specifically focusing on lower limb-BFR training, it shows promise as an efficient alternative that could replace the usual heavy-load approach when heavy load in appropriate, for example after and injury.
Interestingly, the exact mechanisms behind why we see these strength improvements in clinical populations are not yet clear. There isn’t a definitive body of literature that provides a complete explanation.
The idea is that similar processes like muscle growth (hypertrophy) and adaptations in the nerves (neural adaptations), which we observe in heavy-load training, might be the reasons for the differences we see with BFR. The combination of tension and reduced oxygen supply (hypoxia) during BFR exercises is thought to kickstart these processes, providing a unique perspective on how strength gains work in a more nuanced way.

Safety and Effectiveness of blood flow restriction
In the analysis of the 20 studies conducted by Hughes, it’s notable that a significant majority of these studies do not mention any adverse events linked to BFR. This oversight becomes particularly crucial because lower limb-BFR training has proven effective in enhancing various physiological aspects, except for muscle strength. This positions it as a great tool for tackling muscle atrophy, especially during early immobilisation.
Encouragingly, the integration of BFR into low-load training doesn’t seem to worsen conditions or lead to exercise-related pain. This Suggests that incorporating BFR into training protocols may be a safe and effective strategy. Concerns initially raised about potential disruptions in blood circulation and the risk of ischaemic reperfusion injury have been addressed in in-depth reviews. These reviews affirm that when implemented correctly, BFR training poses no greater risk than traditional exercise methods.
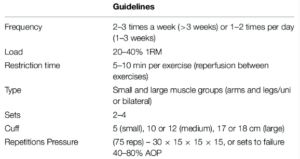
Optimising Blood Flow Restriction Training
To make Blood Flow Restriction training effective, it’s crucial to personalise the prescribed occlusive pressure, a key aspect often overlooked in current literature. There’s a significant gap in individualising this pressure to ensure both the safety and effectiveness of BFR application. Studies in healthy individuals highlight the importance of considering thigh circumference when determining occlusion pressure. Logically, larger limbs need higher pressure to achieve the same occlusion levels as smaller limbs.
A promising method involves calculating Total Arterial Limb Occlusive Pressure (LOP), offering a standardised way to choose pressure as a percentage of LOP for consistent occlusion levels across different muscle sizes. This approach, commonly used in surgery by Registered Nurses to calculate tourniquet pressures, aims to limit blood flow and reduce the risk of adverse events.
Studies using this method challenge the idea that higher LOP pressures always lead to greater muscular responses. Research shows that using 40% of LOP can bring about similar improvements in muscle size, strength, and endurance over an 8-week training period, comparable to those achieved with 90% LOP but with significantly less reported discomfort.
Personalised prescription not only induces sufficient muscle adaptations but also reduces the risk of adverse events and minimises discomfort, which is what we all should be aiming for as clinicians.

Diverse Physiological Benefits of BFR Training
BFR training isn’t just about building muscle strength – it’s a versatile intervention with a range of physiological adaptations. Research indicates that as little as 6 weeks of low-load BFR training can lead to a noticeable increase in serum concentrations of bone alkaline phosphatase. This suggests a positive impact on bone health by promoting increased bone turnover.
In the context of older individuals, incorporating BFR into low-load walking proves to be a helpful approach. This type of training improves various factors such as
- Knee extensor and flexor torque
- Carotid arterial compliance
- Peak oxygen uptake
- Peak post-occlusive blood flow
- Vascular endothelial function
- Peripheral nerve circulation.
This highlights the impact of BFR on multiple physiological parameters, demonstrating the potential to assist overall health and functional capacity in older populations.
The benefits of BFR training go beyond the elderly. It holds promise for clinical groups dealing with musculoskeletal weakness and bone degradation. Conditions like osteoporosis, rheumatoid arthritis, multiple myeloma, and lymphoma may benefit from BFR training as a valuable addition to conventional rehabilitation strategies.





Leave a Reply