
How ankle sprains affect our brain
In the dynamic world of athletics, the prevalence of ankle sprains poses a substantial risk, with an alarming incidence rate of 11.3 ankle sprains per 1000 athlete exposures.
This article aims to delve into the study by Maricot and colleagues and explain the immediate and long-term consequences of ankle sprains, unraveling the intricate impact on ligaments, muscles, and nerves.
From the localised effects such as pain, swelling, and neuromuscular deficits to the enduring challenges manifested in Chronic Ankle Instability, our exploration spans the physiological and neurological realms.
We set the stage for understanding the broader implications and guiding effective rehabilitation strategies for athletes & clinicians grappling with ankle injuries.
Definitions:
There are a lot of words in this article that make the head spin – let’s get some definitions out of the way.
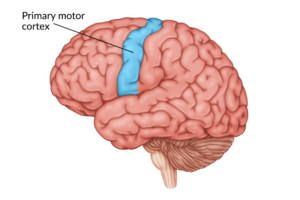
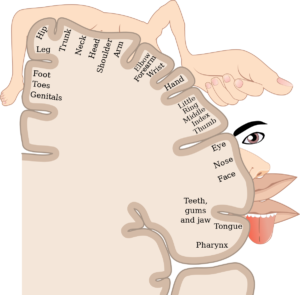
- Corticomotor Excitability: Corticomotor excitability refers to the ability of the motor cortex (the part of the brain responsible for controlling voluntary muscle movements) to generate neural impulses and subsequently induce muscle contractions.
- Corticospinal Inhibition: Corticospinal inhibition is the process by which the motor cortex reduces or inhibits the activity of the corticospinal tract, which is responsible for transmitting motor signals from the brain to the spinal cord and muscles. Inhibition can occur to modulate muscle activity and prevent unwanted movements.
- Corticomotor Output Mapping: Corticomotor output mapping involves the study and representation of the areas of the motor cortex that control specific muscles or movements. It helps in understanding the organization of motor control in the brain.
- Postcentral Gyrus: The postcentral gyrus is a region of the cerebral cortex located in the parietal lobe of the brain. It is primarily responsible for processing somatosensory information, including touch, temperature, and proprioception (sense of body position).
- Afferent Information: Afferent information refers to sensory signals or information that travels from the periphery (e.g., skin, muscles, organs) towards the central nervous system (the brain and spinal cord).
Afferent neurons transmit sensory data for processing.
- Somatosensory Cortex: The somatosensory cortex is a part of the brain, typically found in the parietal lobe, responsible for processing sensory information related to touch, pressure, temperature, and pain. It plays a crucial role in somatosensation.
- Somato-Sensation: Somato-sensation is the collective term for sensory perceptions related to the body’s surface, including touch, temperature, pain, and proprioception.
- Afferent Information Decoupling: Afferent information decoupling refers to the process of separating or altering the transmission of sensory signals within the nervous system. This may be done experimentally or clinically to study or manipulate sensory perception.
- Transcranial Magnetic Stimulation (TMS): Transcranial magnetic stimulation is a non-invasive neurostimulation technique that uses magnetic fields to stimulate specific regions of the brain. It is used for research and therapeutic purposes to modulate brain activity.
- Cortical Silent Period: The cortical silent period is a brief interruption in the electrical activity of the motor cortex that occurs after a voluntary muscle contraction. It is a neurophysiological phenomenon often studied in the context of motor control and neurology
Long-Term Impact of Chronic Ankle Instability and Neurological Changes
Chronic Ankle Instability takes center stage, revealing the lasting effects experienced by patients one year after the initial injury. The aftermath of ankle sprains is marked by persistent symptoms, self-reported disability, and a decrease in physical activity.
The high rates of re-injury can be attributed to changes in the central nervous system. Notably, alterations in both the structure and function of the brain, especially in regions related to motor function, offer valuable insights into the complex interplay between ankle injuries and the broader neural network.
As we unravel the intricate relationship between ankle sprains and neurological changes, the implications for rehabilitation become clear. A comprehensive understanding can guide specific interventions for both immediate and long-term effects of ankle sprains. Healthcare professionals can enhance rehabilitation strategies by addressing not only the localised injuries but also the neural adaptations the follow.
The holistic approach sets the stage for more effective management of ankle sprains.
Here are 3 main changes that can occur after an ankle sprain
Enjoying the article? Get more insights and breakdowns of research studies by signing up to our free weekly newsletter – HERE

Functional Brain Adaptation
The concept of functional brain adaptation involves understanding corticomotor excitability, which essentially reflects how easily neurons in the motor cortex fire signals. This excitability is crucial in controlling various muscles in our body.
Research has found that there is a decrease in corticomotor excitability in specific regions of the primary motor cortex that play a role in managing leg muscles such as the peroneus longus, tibialis anterior, soleus, and gastrocnemius medialis.
This reduced efficiency in communication within the pyramidal tracts, particularly in the primary motor cortex, might contribute to neuromuscular issues affecting postural control. In individuals with chronic ankle instability, there’s evidence suggesting smaller map areas and volumes, indicating more focused clusters of neurons communicating with the peroneus longus muscle.
This concentration of communication might result in motor cells near the peroneus longus border being less dedicated to their specific function, leading other parts of the brain to compensate. This shift in muscle excitability could be a contributing factor to altered movement patterns, potentially increasing the risk of ankle re-injury.
In the context of chronic ankle instability, a decrease in both corticomotor map area and volume may limit the self-organisation capacity of the motor cortex. This limitation in self-organisation could have implications for overall motor control and coordination in individuals with Chronic Ankle Instability.
Sensory Information and the Brain
Let’s break down the concept of how the brain processes sensory information, focusing specifically on feedback from the foot to the brain. In simpler terms, we’re looking at how the brain understands signals from the feet.
Recent research suggests that there are changes in the postcentral gyrus, a region of the brain, because of a decrease in the connection of incoming sensory information.
The extent of this reduction in connection becomes more pronounced as the intensity of the sensory input increases. Essentially, the stronger the stimulus, the more the communication between the foot and the brain seems to be altered.
This alteration in communication could have implications for how our bodies respond to stimuli. Particularly, it might affect our ability to prepare for or react to specific situations, given the importance of the somatosensory cortex in processing information about our body’s position and movement.
The changes observed in sensory receptors and the somatosensory cortex might have consequences for the risk of injury. When proprioception perception is distorted, meaning the brain’s ability to sense the position and movement of joints is affected, it could potentially increase the likelihood of injuries.
The Impact of Fear of Injury
Fear plays a significant role in contributing to the challenges faced by individuals with Lateral Ankle Sprains.
In a study by Xue and colleagues , researchers delved into the neural activity associated with evaluating injury-related situations. They pinpointed a notable deactivation in a region of the limbic system known as the dorsal anterior cingulate cortex.
This deactivation was found to be closely linked to heightened levels of fear. Essentially, individuals with Lateral Ankle Sprains demonstrated reduced activity in this brain region when processing situations related to sprains, and this decrease in activity was associated with an increased sense of fear compared to those without such injuries.
As time progresses, a noteworthy pattern emerges. Initially, individuals with Lateral Ankle Sprains tend to adopt a passive appraisal and avoidance coping strategy as a response to their fear of injury.
However, this approach becomes maladaptive over time.
In practical terms, it means that these individuals start avoiding sports activities altogether due to their persistent fear of (re)injury. This avoidance behaviour becomes a hindrance, contributing to the disability experienced by patients and affecting their overall engagement in physical activities.

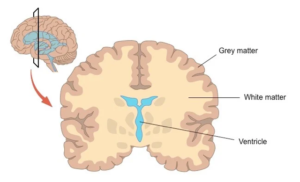
Changes in Brain Structure
So far, we’ve explored how individuals with Chronic Ankle Instability experience challenges in activating their ankle muscles. Now, let’s shift our focus to structural changes in the brain that support the notion of electrophysiological shifts.
Recent evidence points to alterations in the corticospinal tract, a neural pathway connecting the brain to the spinal cord. These structural changes suggest that there are measurable shifts in the electrical activity of the brain in individuals with Chronic Ankle Instability.
When we examine ankle injuries with characteristics similar to those found in Lateral Ankle Sprains, it becomes apparent that these injuries could potentially lead to detrimental changes in the microstructure of white matter.
White matter is crucial for controlling postural stability, and alterations in its microstructure may elevate the risk of experiencing future musculoskeletal injuries.
In essence, these structural adaptations in the brain, particularly in the corticospinal tract, provide further insights into the complex interplay between neural changes and the increased risk of musculoskeletal issues in individuals.
Clinical Implications
In individuals with Chronic Ankle Instability, disruptions in corticomotor pathways can lead to compensatory movements and alterations in joint function. Unfortunately, these adaptations often fall short in preventing recurring Lateral Ankle Sprains, resulting in persistent pain, instability, and limitations in daily activities.
Unlike those who cope effectively (termed “copers”), Chronic Ankle Instability patients exhibit notable functional and structural changes that contribute to reported disability. Copers, on the other hand, show no significant deviations from healthy individuals in terms of function or structure.
For effective rehabilitation, it is crucial to address central adaptations, steering them towards functional outcomes.
Active strategies such as resistance training, proprioception exercises, balance training, and motor learning can potentially alleviate sensorimotor issues and reduce the recurrence.
In the rehabilitation process, it’s essential to take into account the psychological aspect, particularly the fear associated with injury. Patients with effective coping skills are more likely to return to sports compared to those who tend to avoid potentially challenging situations.
Tools like the Injury-Psychological Readiness to Return to Sport Scale can assist clinicians in making well-informed decisions regarding the appropriate timing for a return to sports activities. This comprehensive approach ensures that rehabilitation efforts address both physical and psychological aspects, promoting a more successful recovery.
Final Thoughts
As we navigate through the layers of ankle sprains and their repercussions, the imperative for a comprehensive approach to rehabilitation becomes apparent. Chronic Ankle Instability emerges as a focal point, showcasing how disruptions in corticomotor pathways contribute to persistent issues in joint function. The structural adaptations in the brain, particularly within the corticospinal tract, shed light on the intricate interplay between neural changes and the heightened risk of musculoskeletal problems.
Looking ahead, the implications for rehabilitation extend beyond merely addressing local injuries. A holistic understanding allows healthcare professionals to tailor interventions that encompass both the immediate and long-term effects of ankle sprains. Active strategies, including resistance training, proprioception exercises, and addressing psychological aspects like fear, present promising avenues for mitigating sensorimotor issues and reducing the recurrence of ankle injuries.
In concluding our exploration, we emphasise the importance of ongoing research to uncover novel perspectives and refine rehabilitation protocols. By acknowledging the interconnected nature of physical and neural adaptations, we pave the way for more effective management of ankle sprains in athletic populations, fostering a balance between recovery and a return to optimal sports performance.
Credit
- Maricot, A., Dick, E., Walravens, A., Pluym, B., Lathouwers, E., De Pauw, K., Verschueren, J., Roelands, B., Meeusen, R. and Tassignon, B., 2023. Brain Neuroplasticity Related to Lateral Ankle Ligamentous Injuries: A Systematic Review. Sports Medicine, pp.1-21.
- Xue, X.A., Li, S., Li, H., Li, Q. and Hua, Y., 2021. Deactivation of the dorsal anterior cingulate cortex indicated low postoperative sports levels in presurgical patients with chronic ankle instability. BMC Sports Science, Medicine and Rehabilitation, 13, pp.1-9.





Leave a Reply