
Diagnose & treat jumpers knee effectively
This article provides essential insights in the world of patellar tendinopathy. It encompasses assessment techniques, effective management strategies, and valuable tips, serving as a comprehensive resource for your academic and practical pursuits in the field of sports medicine.
Explore this article to enhance your understanding, make informed decisions in your practice, and take proactive steps towards addressing tendinopathy related issues in the general and athletic setting.
Have fun!
Check out our article that delves into the symptoms, healing time and facts about patellar tendinopathy – Here
5 Key takeaways of the article
- Comprehensive History is Vital: Gathering a thorough patient history, including pain location and past treatments, is crucial to identify the source of patellar tendinopathy.
- Functional Assessments: Functional tests like the single-leg decline squat helps to pinpoint pain and assess tendon-bone junction involvement.
- Exercise-Based Management Works: Eccentric exercises, such as single-leg decline squats, can effectively relieve symptoms and improve tendon health.
- Progressive Return to Sport: Focus on gradually reintroducing high-load activities and sports-specific training to ensure a safe and successful return to sport.
- Patient Education is Critical: Educate patients about symptom monitoring, realistic expectations, and the importance of maintaining strength exercises for long-term tendon health.
How to assess patellar tendinopathy
History Taking
Gathering a comprehensive history is a fundamental step in assessing and managing patellar tendinopathy. It serves as a critical initial step in determining whether the patellar tendon is indeed the source of pain.
Below are some questions to consider:
Onset of Symptoms:
- When did the pain begin?
- Was there a specific incident or gradual onset?
Nature of Pain:
- Describe the pain (sharp, dull, throbbing, etc.).
- Is the pain constant or intermittent?
- Does the pain worsen with specific activities or movements?
Location and Radiation:
- Where is the pain located around the knee?
- Does the pain radiate to other areas?
Aggravating and Alleviating Factors:
- What activities or movements aggravate the pain?
- Are there specific positions or interventions that alleviate the pain?
Activity Level and Sports Participation:
- Inquire about the patient’s level of physical activity.
- Ask about any specific sports or exercises that may contribute to the symptoms.
Training Intensity and Changes:
- Explore any recent changes in training intensity or frequency.
- Have there been alterations in the training regimen or equipment?
Previous Injuries and Treatment:
- Ask about any previous knee injuries or treatments.
- Explore the effectiveness of previous interventions.
Occupational and Daily Activities:
- Assess the impact of daily activities and occupation on the symptoms.
- Inquire about prolonged sitting or standing.
Mechanical Symptoms:
- Ask about any mechanical symptoms such as locking, popping, or giving way.
- Explore if there are any issues with joint stability.
Rehabilitation and Exercises:
- Explore any current or past rehabilitation programs.
- Inquire about specific exercises that may have been prescribed.
- Consider psychological aspects, such as stress and emotional well-being.
- Explore the impact of symptoms on daily life and mental health.
Functional Limitations:
- Assess any limitations in daily activities or range of motion.
- Explore how the symptoms affect the patient’s overall function.
Timeline of Symptoms:
- Establish a timeline of symptom progression.
- Identify any patterns or fluctuations in the severity of symptoms.

Pain Localisation:
Ask the patient to pinpoint the exact location of their pain within the patellar region. If the pain is distributed more broadly, this may raise suspicions of alternative diagnoses.
Identifying the Cause:
Understanding the reason behind the development of painful tendons is crucial. This typically stems from tendon overload, which can manifest in two common scenarios:
- A sudden increase in overall load, such as starting plyometric training or participating in a high-volume tournament
- Returning to regular training after a significant period of inactivity, like resuming training after a 4 to 6-week break due to factors like an ankle sprain or holidays.
Pain Behaviour & triggers
Patellar tendinopathy often exhibits characteristic pain behaviour. Symptoms may include initial soreness at the start of physical activity, variable responses to warm-up (ranging from complete relief to no relief), and exacerbation of pain on the following day, which can persist for several days.
Patients may report discomfort during prolonged sitting, particularly in a seated position in a car. This pain during sitting can serve as a useful indicator of improvement as the condition progresses.
Activities such as climbing stairs and squatting are known to provoke pain in individuals with patellar tendinopathy. Most patients who present with this condition tend to be proficient power athletes, excelling in activities like jumping and quick changes of direction.
Previous Treatment:
Documenting the patient’s history should include a thorough record of all prior treatments they have tried, including different interventions and rehabilitation strategies. This documentation should encompass both successful and unsuccessful interventions, along with specifics such as exercise details (repetitions, sets, weights, and frequency).
Knowing this information will help you structure your treatment plan. Make sure to note how compliant they were with the previous plan as this will give you a chance to explain and educate the importance of adherence (i.e tendon load) to the tendon healing.
Enjoying the article? Have a look at our analysed studies – HERE
Objective examination
Baseline Measurement:
Establishing a baseline is crucial, and one valuable tool is the VISA-P questionnaire. This assessment tool gauges symptoms, evaluates basic functional tests, and assesses the ability to participate in sports.
It employs a visual analogue scale (VAS) with scores ranging from 0 to 10, with 10 representing optimal health. Scores below 80 indicate dysfunction, while a fully functioning athlete scores 100. Regular monitoring with this questionnaire is advisable, with a minimum clinically significant change of 13 points.
Tenderness on Palpation:
Tenderness on palpation is not a reliable diagnostic technique and should be avoided as an outcome measure.
Muscle Wasting:
Observation often reveals muscle wasting in the quadriceps and calf muscles, particularly the gastrocnemius, compared to the unaffected side. Consider, Using a circumference measure to determine if change in muscle bulk correlates with symptom reduction.
This is not essential, thus use your own clinical judgement.
Clinical Tests:
The single-leg decline squat:
It’s a key clinical test which involves squatting on the affected leg on a 25-degree decline board while maintaining an upright trunk. The test is also conducted on the unaffected leg. The angle of knee flexion and the level of pain on a visual analogue scale are recorded.
Pain during this test should typically remain confined to the tendon-bone junction.

Functional Assessment:
- Single-leg hop tests
- change-of-direction tasks
These can help assess the quality of movement, with pain and function noted during take-off and landing. Evaluating whether increased load induces more pain is important.
Muscle Strength & endurance
Assessing lower leg strength & endurance through clinical and functional measures, such as repeated calf raises and decline squats or handheld dynameter for strength, can provide insights into unloading in essential muscle groups.

Dorsiflexion Range of Movement:
Evaluating ankle dorsiflexion ROM is critical, as the ankle and calf play a significant role in absorbing landing energy. Stiffness in the talocrural joint dorsiflexion, general foot stiffness, or hallux rigidus can contribute to increased load on the leg’s musculotendinous complexes.
How to fully test the knee for tendinopathy
Distinguishing between patellar tendinopathy and “general” knee pain is crucial for effective treatment. When assessing the knee, consider the role of movement patterns.
Begin with basic functional exercises tests like:
- Squats
- Single-leg squats
Pay attention to weight distribution, excessive forward leaning, toes raising up etc. during the movements and identify which one provokes more pain.
If there’s compensation during these tasks look into,
- Ankle mobility
- Tibial rotation
- Hip internal and external rotation
To specifically test for tendinopathy, remember that it’s often load-related and worsens with rapid use. Conduct a series of dynamic movements such as:
- Double-leg jumps 5x
- Single-leg jumps 5x
And assess the discomfort experienced. If the jumps provoke more pain, it’s likely related to tendinopathy. Conversely, if squats and single-leg squats are more painful, it may be due to mobility or biomechanics issues.
Early management of patellar tendinopathy
Patellar tendinopathy is a condition characterised by persistent changes within the patellar tendon. While complete resolution of these structural changes may not always be achievable, the focus of management is primarily on alleviating symptoms.
Conservative approaches are typically employed to achieve this goal.
The intervention strategy for patellar tendinopathy is multifaceted. Initially, the emphasis is on pain reduction. This is followed by a progressive exercise program designed to address strength deficits, enhance the capacity of the tendon in the stretch-shorten cycle, and eventually facilitate a safe return to sport-specific activities.
Pain Reduction:
Managing an athlete’s symptoms involves careful load management. It is crucial to avoid complete cessation of activities that load the tendon, as this can further decrease its capacity to tolerate stress.
Instead,
- Reduce high-load drills
- Decrease in training frequency (often twice a week is sufficient)
- Reduce training volume (shortening training duration)
These recommended strategies aim to lessen the load on the tendon without necessitating complete rest.
Isometric Contractions:
Sustained isometric contractions such as wall sits, Spanish squats or squat holds on a 25 degree wedge, held at 70% of a persons maximum for 45 to 60 seconds and repeated 4 times, has shown analgesic effects and can be incorporated into the loading strategy.
Other treatment options for patellar tendinopathy
Manaual therapy
While passive treatments for patellar tendinopathy are sometimes employed, there is limited evidence supporting their effectiveness.
Among passive interventions, exercises have demonstrated the most favourable outcomes in both the short and long term.
Manual therapy techniques, such as myofascial manipulation of the knee extensor muscle group (Quads), have also shown positive results in reducing pain for patellar tendinopathy patients in both short-term and long-term follow-up.
Manual therapy are generally best employed to alleviate symptoms rather than as primary treatments.
Taping
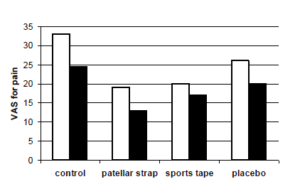
A study dove into the world of athletes dealing with patellar tendinopathy. The researchers wanted to find out if strapping the patellar or using sports tape could actually make a difference.
The study found that athletes using these supports experienced significantly less pain, especially during tough activities like the single leg decline squat. The patellar strap and sports tape decreased the pain scores by over 12 points in the VAS pain scale.
Interestingly, it seems like females get even more relief from sports tape compared to the males. More research is needed to see if these effects hold up in the heat of actual sports action.
Shockwave Therapy:
When it comes to shockwave there is mixed results, Here is conclusions of the followig studies. I encourage you to have a read and decide what is best for your practice.
Zwerver et al 2011 randomised control trial on athletes
“Using shockwave therapy as the sole treatment for actively competing athletes with patellar tendinopathy, who have experienced symptoms for less than 12 months, does not provide any advantages over a placebo treatment during the competitive season.”
Rudavsky, A. and Cook, J., 2014 a review of the literature
“Shockwave Therapy appears to be a promising and safe option for treating patellar tendinopathy, showing positive outcomes in terms of pain relief and improved function.
However, it’s important to note that, as of now, twe cannot provide a specific recommended treatment protocol due to the current state of knowledge in this field”
Charles et al 2023 – systematic review & meta-analysis
“This meta-analysis found that the effectiveness of shockwave therapy varies person to person. Shockwave had minimal impact on short-term pain and function for patellar tendinopathy compared to placebo or placebo + eccentric exercise.
However, shockwave significantly reduced pain compared to conservative treatment (various types, I suggest to have a look at the study) for patellar tendinopathy”
Corticosteroid Injections:
Corticosteroid injections, oral steroids, and iontophoresis are options for reducing pain and inflammation in reactive tendons.
They can bring quick relief, but it’s important to know that they don’t provide long-term results as good as exercise-based approaches. Corticosteroid injections may not be effective for degenerative tendinopathy cases and are generally discouraged.
Analgesic injections, in general, should be used cautiously, especially during the active season, as they may mask symptoms and lead to overexertion with poorer outcomes.
Exercise based management for patellar tendinopathy
Strengthening Exercises
Eccentric exercises have demonstrated positive outcomes in both short-term symptom relief and long-term improvements in VISA-P scores (a measure of patellar tendinopathy severity).
One effective exercise is the single-leg decline squat at a 25-degree angle, which offers better results than a standard single-leg flat squat. This effectiveness is attributed to the increased moment arm of the knee achieved by using a decline board.
However, it’s important to note that eccentric exercises may not always be beneficial during a competitive season, as they could potentially worsen symptoms or injury risk, particularly in athletes already engaged in high-load activities.
Additionally, a combination of exercises involving eccentric, concentric, and plyometric training has been explored, showing promise for rehabilitation in patellar tendinopathy cases.
When dealing with a patellar tendinopathy follow a 3 stage protacol
Exercise ideas & their progressions:
Quads
- Body weight squat (3/20) – Split squat (3/15) – weighted elevated split squat(3/8-15)
- Step down (3/20) – later step down (3/20) – elevated step down (3/8-15)
Hamstring
- Eccentric double leg slider (3/12) – Double leg slier (3/12) – Single leg eccentric (3/8) – single leg slider (3/8)
- Single leg RDL hand supported (3/3/6-12 – Single leg RDL bodyweight – weighted
Glute/trunk
- Short side plank (3/60 sec) – side plank (3/60sec) – side plank hip abduction (3/45-60 sec)
- Double leg bridge (3/20) – single leg bridge ( 3/15) – single leg hip thrust (3/12-15)

Returning to Sport after jumpers knee
Functional strengthening plays a pivotal role in an athlete’s return to sport after patellar tendinopathy. This involves addressing the tendon’s high-load capacity, as well as addressing kinetic chain deficits and movement patterns.
Once these fundamentals have improved, the athlete can begin sports-specific training. The progression towards faster contractions is essential, as it mimics the stretch-shorten cycle, forming the foundation for returning to sports.
Early drills should include activities like
- Skipping
- Jumping
- Hopping
- Gradually advancing to agility tasks
- Direction changes
- Sprinting, and bounding movements.
Quantifying and categorising these tasks using a high-low-medium-load approach is advisable during the reintroduction of high-load activities.
Key points to consider for patellar tendinopathy
Education:
- Realistic Expectations:
Athletes/Patients need to have realistic expectations about their rehabilitation process and understand that managing symptoms is an ongoing requirement throughout their activities/sports career, whether they’re recreational or professional.
- Monitoring and Adjustments:
Individuals must learn how to monitor their symptoms and make appropriate adjustments to their participation and loading during rehabilitation and when returning to sports. Maintaining strength exercises twice a week is crucial for long-term tendon health.
- Delayed Response:
Tendons often respond to load with delayed pain, typically emerging about 24 hours after activity. People should be prepared for this and not be alarmed by minimal pain during physical activity.
- Self-Assessment:
The single-leg decline squat is an effective self-assessment tool to monitor symptoms and gauge response to rehabilitation. Prepose for people to keep a journal of symptoms and pain during this exercise can help identify triggers and manage symptoms independently.
Factors Affecting Prognosis:
- Severity and Dysfunction:
The speed of return to sport depends on the severity of pain and dysfunction, the quality of rehabilitation, and various intrinsic and extrinsic factors. Athletes/patients with significant kinetic chain dysfunction may take 6 to 12 months to recover muscle and tendon capacity, regardless of pain levels.
- Sport-Specific Demands:
Athletes aiming to return to high-level performance should consider the specific demands of their sport. For example, an elite high jumper may require more extensive rehabilitation than a recreational football player due to differing athletic requirements.
- Sport Variations:
Even within elite sports, the loading demands on the patellar tendon can vary significantly. Athletes in sports like volleyball, which involve frequent jumping and landing, may need more extensive rehabilitation compared to those in sports like hockey.
Factors Affecting Response to Therapy:
- Pain Complexity:
The exact nature of pain in tendinopathies is not fully understood. Emerging evidence suggests a potential link to central sensitization or heightened activity in the central nervous system.
- Mechanical Pain Threshold:
Some studies indicate that athletes with patellar tendinopathy may have a lower mechanical pain threshold and increased sensitivity to certain stimuli, such as vibration disappearance, compared to non-injured athletes.
Other conditions to be aware of
| Name | Symptom | Differentiation |
| Plica or Fat Pad Syndrome: | Include anterior knee pain, swelling, crepitus, pain with knee movement, and tenderness, often linked to irritation of the synovial plica or the fat pad under the patella | its characterised by localised pain and swelling around the patella due to irritation of the synovial plica or the fat pad beneath the patella. It is distinguished by these specific symptoms and can be diagnosed through imaging studies such as MRI. |
| Patellar Subluxation Problem | Characterized by recurrent patella subluxations, it presents with knee instability, pain, swelling, limited range of motion, and joint effusion | Patellar subluxation involves recurrent episodes of the patella partially moving out of its normal position, causing knee instability, pain, and swelling |
| Osgood-Schlatter Disease: | Affecting adolescents during growth spurts, it causes pain, tenderness, swelling, and a visible bump at the tibial tuberosity, usually improving with conservative treatments like rest, ice, and activity modification | It primarily affects adolescents
and usual has a visible bump at the tibial tuberosity at the font of the knee. |
| Patellofemoral Pain Syndrome (PFPS) | Pain around or behind the kneecap, especially when climbing stairs, squatting, or sitting for extended periods | PFPS is more focused on the kneecap area, whereas patellar tendinopathy involves pain at the tendon or at the attachment/origin site below the kneecap. |
| Osteoarthritis | Gradual onset of knee pain, stiffness, and reduced range of motion. Pain is often worse with activity and improves with rest | Osteoarthritis typically affects older individuals and is characterized by joint degeneration, whereas patellar tendinopathy is often seen in younger, active individuals and involves tendon inflammation. |
| Iliotibial (IT) Band Syndrome | Pain on the outer side of the knee or thigh, which worsens with running or activities involving repetitive knee flexion and extension. | IT band syndrome involves pain on the outer side of the knee, whereas patellar tendinopathy typically focuses on the front of the knee. |
| Meniscal Tears | Pain, swelling, and a feeling of catching or locking in the knee, often resulting from a twisting injury | Meniscal tears often involve mechanical symptoms like catching or locking, whereas patellar tendinopathy typically presents with pain during activity. |
| Anterior Cruciate Ligament (ACL) Injury | Sudden onset of pain, swelling, and instability in the knee, often associated with a traumatic event | ACL injuries result from trauma and can cause significant instability, whereas patellar tendinopathy is usually due to overuse and doesn’t typically involve instability. |
| Bursitis | Swelling and tenderness around the knee, often with warmth and redness, especially when kneeling or putting pressure on the knee | Bursitis typically presents with localized swelling and inflammation, whereas patellar tendinopathy is more focused on the tendon area below the kneecap. |
| Rheumatoid Arthritis | Joint pain, swelling, and stiffness that can affect multiple joints, including the knee | Rheumatoid arthritis is an autoimmune condition that affects multiple joints, whereas patellar tendinopathy primarily involves the knee’s tendon and is often due to overuse |
Summary of article
Assessment:
- Gather a detailed history to pinpoint the source of pain in the patellar region.
- Assess pain location, identify the cause (often tendon overload), and note pain behaviour and prior treatments.
Examination:
- Use the VISA-P questionnaire for baseline assessment.
- Avoid relying on tenderness for diagnosis.
- Observe muscle wasting, conduct clinical tests, and assess muscle strength, endurance, and ankle mobility.
Testing for Tendinopathy:
- Distinguish between patellar tendinopathy and general knee pain by analysing movement patterns during squats and jumps.
Acute Management:
- Focus on symptom relief through conservative approaches.
- Manage load carefully, consider isometric contractions, and use passive interventions judiciously.
Return to Sport:
- Focus on functional strengthening and gradual sports-specific training.
Key Points:
- Educate patients on realistic expectations, symptom monitoring, and strength exercises.
- Understand the delayed pain response in tendons.
- Use the single-leg decline squat as a self-assessment tool.
- Prognosis depends on various factors, including severity and sport-specific demands.
- Consider mechanical pain thresholds and central sensitization in treatment response.
Sources
- Charles, R., Fang, L., Zhu, R. and Wang, J., 2023. The effectiveness of shockwave therapy on patellar tendinopathy, Achilles tendinopathy, and plantar fasciitis: a systematic review and meta-analysis. Frontiers in Immunology, 14
- de Vries, A., Zwerver, J., Diercks, R., Tak, I., van Berkel, S., van Cingel, R., van der Worp, H. and van den Akker‐Scheek, I., 2016. Effect of patellar strap and sports tape on pain in patellar tendinopathy: a randomized controlled trial. Scandinavian journal of medicine & science in sports, 26(10), pp.1217-1224.
- Rio, E., Kidgell, D., Purdam, C., Gaida, J., Moseley, G.L., Pearce, A.J. and Cook, J., 2015. Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. British journal of sports medicine, 49(19), pp.1277-1283.
- Rudavsky, A. and Cook, J., 2014. Physiotherapy management of patellar tendinopathy (jumper’s knee). Journal of physiotherapy, 60(3), pp.122-129
- van Leeuwen, M.T., Zwerver, J. and van den Akker-Scheek, I., 2009. Extracorporeal shockwave therapy for patellar tendinopathy: a review of the literature. British journal of sports medicine, 43(3), pp.163-168.
- Zwerver, J., Hartgens, F., Verhagen, E., van der Worp, H., van den Akker-Scheek, I. and Diercks, R.L., 2011. No effect of extracorporeal shockwave therapy on patellar tendinopathy in jumping athletes during the competitive season: a randomized clinical trial. The American journal of sports medicine, 39(6), pp.1191-1199.






Leave a Reply