
Lateral Ankle Sprains – The Ultimate Overview
Did you know that repetitive lateral ankle sprains can lead to chronic symptoms and long-term impairments? With up to 75% of cases resulting in chronic symptoms and a significant likelihood of re-injury, understanding lateral ankle sprains is crucial for both high level athletes and people engaging in physical activity.
By exploring the anatomy, mechanisms of injury, clinical presentation, and risk factors associated with lateral ankle sprains, we can develop effective preventive strategies and improve patient outcomes.
In this article, we will delve into the overview of the lateral ankle sprain and determine key factors to look out for. By gaining a comprehensive understanding of this common injury, you will be able to enhance your knowledge and provide better care to patients, promoting ankle stability and reducing the incidence of sprains.
So, let’s explore the world of lateral ankle sprains and discover how we can prevent and manage this prevalent injury.
5 key takeaways
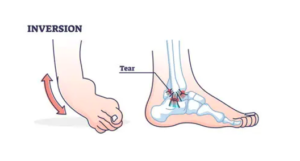
- Lateral ankle sprains involve tears or disruptions of ligaments on the outer aspect of the ankle, often caused by twisting or rolling.
- Repetitive lateral ankle sprains are common, with up to 75% leading to chronic symptoms, yet many individuals do not seek treatment.
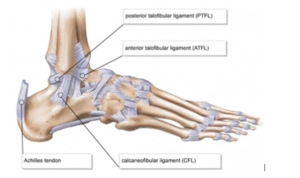
- Ligaments involved include the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior talofibular ligament (PTFL).
- Mechanisms of injury include forceful ankle plantar flexion and inversion, frequently affecting the ATFL.
- Healing time varies by strain severity, imaging techniques can aid in diagnosis, and surgery is considered for severe cases or persistent instability. Risk factors include previous ankle sprains, shoe selection, and fatigue during physical activity.
What is a lateral ankle sprain?
Clinically, a lateral ankle sprain occurs when there is a partial or complete tear or disruption of the ligaments located on the outer aspect of the ankle, most frequently the anterior talofibular ligament and/or calcaneofibular ligament. Patients may present with pain, swelling, and discomfort experienced on the outer side of the ankle, often resulting from an ankle twist or roll.
Fun Facts
- Repetitive lateral ankle sprains (LAS) following the initial injury are very prevalent, with a high percentage (up to 75%) of cases leading to chronic symptoms.
- Due to the perceived lack of importance of LAS in society, approximately 55% of individuals who sustain an ankle sprain do not seek treatment from a healthcare professional.
- A considerable proportion (up to 70%) of patients will experience repetitive LAS and chronic symptoms after the initial injury.
- About 66% of LAS cases involve isolated injury to the anterior talofibular ligament (ATFL), while both ATFL and calcaneofibular ligament (CFL) ruptures occur concurrently in another 20%.
- Chronic ankle instability (CAI) not only limits physical activity but also contributes to the degeneration of the talus joint and increases the risk of osteoarthritis
Study: Link
Ankle joint anatomy
The lateral aspect of the ankle is protected by three ligaments’, the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL) and the posterior talofibular ligament (PTFL).
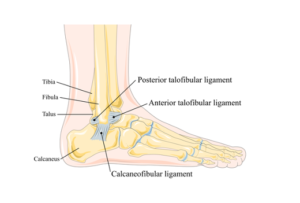
Origin:
- ATFL: Originates from the anterior aspect of the lateral malleolus, which is the bony prominence on the outer side of the ankle.
- CFL: Originates from the lateral (outer) and inferior (lower) aspect of the fibula malleolus.
- PTFL: Originates from the posterior (back) aspect of the lateral malleolus
Insertion:
- ATFL: inserts onto the talus bone
- CFL: The CFL inserts onto the lateral (outer) aspect of the calcaneus bone (lateral tubercle)
- PTFL: inserts onto the posterior (back) aspect of the talus bone (posterior tubercle)
Function:
- ATFL: The ATFL is the most commonly injured ligament in the ankle. It plays a crucial role in resisting excessive inversion (inward rolling) of the foot, which is a common mechanism of lateral ankle sprains. It provides stability to the ankle joint, particularly during activities involving rapid changes in direction and sudden movements.
- CFL: it primarily resists inversion forces, preventing excessive inward rolling of the foot. The CFL provides additional support to the ankle, especially when the foot is in a plantarflexed (toes pointed downward) position.
- PTFL: It plays a role in limiting excessive backward movement (plantarflexion) of the foot. It provides stability to the ankle by restraining excessive posterior displacement of the talus bone, ensuring proper alignment and preventing injuries during activities involving forceful plantarflexion.
These ligaments work in concert to maintain the stability and integrity of the ankle joint, preventing excessive movements that could lead to sprains or other injuries. When all these ligaments are healthy and functioning properly, they help provide stability and support during weight-bearing activities, allowing for efficient movement and reducing the risk of ankle instability.
Mechanism of injury for lateral ankle sprain
Forceful ankle plantar flexion and inversion are the most common mechanisms of injury that often result in tearing of the lateral ligaments of the ankle either in sport or accidental such as slipping of a side curb or walking in high heels.
Specifically, as mentioned previously the anterior talofibular ligament (ATFL) is the most frequently affected. When the ATFL is strained, it is typically followed by damage to the calcaneofibular ligament (CFL), and in very rare cases, the posterior talofibular ligament (PTFL).
Epidemiology – The prevalence of LAS
Lateral ankle sprains are highly prevalent injuries, particularly among athletes and people who engage in sport such as running, jumping, or sudden changes in direction like basketball.
The epidemiology of lateral ankle sprains includes the following key points:
Incidence:
It’s one of the most common injuries, accounting for a significant proportion of all ankle injuries. The exact incidence can vary depending on the population studied and the level of activity the person does. Studies have reported incidence rates ranging from 2 to 35 sprains per 1,000 person-years or discussed by Bridgman et al, 52.7 per 10,000 people
Age and Gender:
Lateral ankle sprains can occur at any age, but they are most common in young active adults and athletes. The incidence tends to be higher in males during adolescence and early adulthood, likely due to higher participation rates in sports and higher-risk activities. However, in older adults, the incidence of ankle sprains tends to be higher in females, possibly due to factors such as decreased muscle strength and balance as well as combining alcohol and high heels on a night out .
Sports Participation:
They are frequently associated with explosive activities or freak accidents. Sports that involve jumping, cutting, and sudden changes in direction, such as basketball, football, volleyball, and tennis, have higher rates of ankle sprains. Athletes involved in these sports often experience lateral ankle sprains due to the high demands placed on the ankle joint.
Get free analysed research studies straight to your inbox: Sign up here
The clinical presentation of a lateral ankle sprain
Patients with lateral ankle injuries commonly present with the following clinical symptoms:
- Pain experienced on the lateral aspect of the foot, specifically around the ankle joint. This pain is often exacerbated by weight-bearing activities and movements involving ankle motion. Swelling and bruising around the affected area are frequently observed.
- Swelling occurs due to the inflammatory response triggered by the injury, while bruising may result from blood vessel damage.
- Loss of range of motion (ROM) are commonly reported by patients. This may be due to pain, swelling, and/or neuromuscular guarding of the injured ankle by the nervous system. Reduced ROM usually is usually seen after injury has heeled thus it’s important to assess at follow ups.
- Increased ankle laxity, instability or excessive joint mobility can be observed during physical examination . Patients may complain of recurrent episodes of their ankle giving way or feeling unstable, indicating ligamentous laxity resulting from the injury. Instability refers to a subjective feeling of the ankle being unreliable or giving way, which can significantly impact confidence and activities of daily living.
Time frame of healing
The duration of healing for ligament strains varies depending on the severity of the injury. However, as a general rule of thumb, the following timelines can be seen:
Grade 1 Strain: Typically, Grade 1 injury involves mild stretching or microscopic tears of the ligament fibres. In most cases, these strains heal within a relatively short period, ranging from 1 to 14 days. With appropriate management and rehabilitation, patients can expect a quick recovery.
Grade 2 Strain: Grade 2 injury involves a moderate level of ligament fibre tearing. The healing process for these strains generally takes longer than Grade 1 strains. Patients can expect a healing timeframe of around 14 to 21 days. Tailored rehabilitation, including exercises to promote stability and strength, is crucial to optimize healing and restore normal function.
Grade 3 rupture: Grade 3 strains are the most severe, involving complete ligament tears or significant disruption. Healing for Grade 3 strains is a more prolonged process compared to lower-grade strains. Typically, patients should anticipate a healing period of approximately 6 to 12 weeks. Rehabilitation for Grade 3 strains is critical to regain stability, strength, and function in the affected joint and prevent chronic ankle instability.
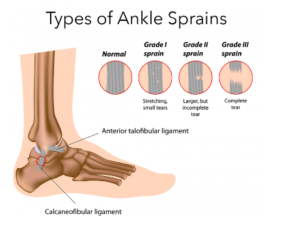
It is important to note that these timelines are general estimates and can vary among individuals depending on factors such as overall health, diet, adherence to rehabilitation protocols, and the demands placed on the injured ligament, for example is a person needs to return to a job that requires a large amount of weight bearing.
The role of imaging in lateral ankle sprains
Imaging plays a valuable role in determining the extent and severity of ankle sprains, particularly in cases where the diagnosis is uncertain, or when there is suspicion of other structural damage such as bone breaks.
Whilst most ankle sprains can be diagnosed clinically based on the history, physical and subjective assessments, imaging can provide additional information that help guide treatment decisions. Dependent on the grade of the sprain a different treatment protocol will be followed, thus it’s beneficial to determine the severity to provide the best treatment plan.
Most ankle sprains will not need MRI imaging, however x-rays are crucial to guide the treatment.
X-ray:
They are typically performed first in ankle injuries to rule out fractures and assess the alignment of the bones. It can identify fractures or avulsion injuries, which may require different treatment approaches than a simple sprain. X-rays are particularly important if there is significant pain, inability to bear weight, or if the mechanism of injury suggests the possibility of a fracture.

Magnetic Resonance Imaging (MRI):
MRI is a valuable imaging modality for ankle sprains, especially when there is suspicion of associated soft tissue injuries, ligament tears, or if the clinical examination findings are inconclusive. MRI can provide detailed images of the ligaments, tendons, cartilage, and other soft tissues, helping to identify any tears, damage, or inflammation.

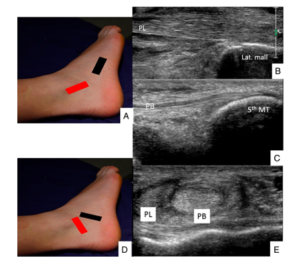
Ultrasound:
Ultrasound is a dynamic imaging modality that can be used to assess ligament integrity, identify fluid collections (such as hematomas), and evaluate tendon injuries. It can provide real-time visualization and can be used for guided injections or to assess healing progress during rehabilitation. Ultrasound is particularly useful in certain clinical scenarios, such as when assessing children or if MRI access is limited.
Computed Tomography (CT) Scan:
CT scans may be employed in cases where a fracture or bony injury is suspected but not adequately visualized on X-rays. CT scans provide detailed images of the bones and can assist in detecting subtle fractures, bone displacements, or other complex bony injuries.

Is surgery necessary after a lateral ankle sprain?
Surgery for lateral ankle sprains is generally reserved for cases that involve severe ligament damage or when conservative treatments fail to provide adequate relief or stability. The decision to pursue surgery is typically based on several factors, including the extent of injury, functional impairment, instability, and the individual’s goals and lifestyle.
Here are some considerations regarding when surgery may or may not be necessary for lateral ankle sprains:
When Surgery May Be Necessary:
- Complete Ligament Tear: If the lateral ankle ligaments (such as the ATFL and CFL) are completely torn or severely damaged, surgery may be considered to repair or reconstruct the ligaments. This is more likely in cases where there is persistent instability, recurrent sprains, or significant functional limitations.
- Chronic Ankle Instability: If conservative treatments, such as physical therapy, bracing, and rehabilitation exercises, have been unsuccessful in addressing chronic ankle instability, surgery may be considered. Chronic ankle instability refers to persistent feelings of giving way, recurrent sprains, or persistent pain and functional limitations.
- Athletes or Individuals with High Demands: Surgery may be recommended for individuals who participate in high-demand sports or activities that require a high level of ankle stability, such as professional athletes. Surgical intervention can help restore stability and reduce the risk of further injuries in these cases.
When Surgery May Not Be Necessary:
- Grade 1 and 2 Sprains: Most mild to moderate lateral ankle sprains can be effectively managed with conservative treatment measures, such as initial rest, compression and elevation, physical therapy, and rehabilitation exercises. Surgery is typically not required for these types of sprains, as they often heal with appropriate non-surgical interventions.
- Adequate Healing and Stability: If conservative treatments lead to symptom reduction and visible progression no matter how small, stability, and functional recovery, surgery may not be necessary. In cases where the ligaments heal well, the ankle is stable, and the individual can return to their desired activities without significant limitations, surgical intervention is not necessary.
- Lack of Persistent Symptoms: If person symptoms, such as pain, swelling, and instability, resolve with treatment and do not significantly impact their daily activities or quality of life, surgery is not considered.
It’s important to note that the decision to undergo surgery for a lateral ankle sprain is individualised and should be made in consultation with an orthopaedic specialist or foot and ankle surgeon. They will assess the specific characteristics of the injury, the individual’s goals and expectations, and consider other relevant factors to determine the most appropriate course of treatment. Physiotherapist can make recommendations and refer if necessary thus knowing the signs are important.
Risk factors for sustaining a lateral ankle sprain
Several factors play a role in the occurrence of lateral ankle sprains (LAS) among patients & athletes, and understanding these factors can guide preventive strategies:
Previous Ankle Sprain History:
Patients with a history of previous LAS are at a higher risk of re-injury. However, research has shown that individuals who wear ankle braces or use taping techniques have a lower incidence of LAS compared to those who do not. These supportive measures provide added stability and restrict excessive ankle movement, thereby reducing the risk of sprains.
It’s also important to note that wearing bracing and/or tapping is an external crutch to your foot and thus will increase the ankles dependability on such support. It’s recommended to use bracing/tapping for full effort training sessions or competitive matches, these have the highest risks for sustaining an ankles injury. Warmups, rehab and light training session should be done without external support to enhance tissue adaptation and thus recovery from injury.
Shoe Selection:
The type of footwear worn can significantly impact ankle protection.
Shoes with enhanced ankle support, such as high-top or lace-up designs, offer additional stability and limit excessive ankle motion. By providing a more secure fit and restricting unwanted movements, these shoes can help prevent ankle sprains during sport.
Duration and Intensity of Physical Activity:
The duration and intensity of exercise or competition can influence the likelihood of ankle sprains. Prolonged and intense physical activity can lead to muscle and tendon fatigue, impairing their ability to support and protect the ankle joint effectively. As fatigue sets in, the muscles and tendons may become less capable of providing adequate stability, increasing the risk of ankle sprains. Conditioning and monitoring of fatigue levels can help mitigate this risk.
By considering the risk factors, physiotherapists can develop prevention and rehabilitation strategies to reduce the incidence rates of LAS. Encouraging the use of ankle braces or taping, educating patients about appropriate footwear choices, and implementing fatigue management techniques can contribute to enhanced ankle stability and a lower risk of sprains.

Summary of article
- Repetitive lateral ankle sprains (LAS) often lead to chronic symptoms, with up to 75% of cases resulting in chronicity, and approximately 70% of patients experiencing repetitive LAS.
- LAS is commonly caused by forceful ankle plantar flexion and inversion, most frequently affecting the anterior talofibular ligament (ATFL).
- Lateral ankle sprains are prevalent among athletes and individuals engaging in activities with sudden changes in direction, such as basketball.
- Clinical symptoms of LAS include pain, swelling, loss of range of motion, and increased ankle laxity or instability.
- Healing time varies depending on the severity of the strain, with Grade 1 strains typically healing within 1-14 days and Grade 3 strains requiring 6-12 weeks.
- Imaging techniques such as X-rays, MRI, ultrasound, and CT scans can provide additional information to guide treatment decisions for ankle sprains.
- Surgery for lateral ankle sprains is considered in cases of severe ligament damage, chronic ankle instability, or high-demand activities.
- Risk factors for LAS include a history of previous ankle sprains and inadequate ankle support, while proper shoe selection and managing fatigue levels can help prevent sprains.
Sources
- Bridgman, S.A., Clement, D., Downing, A. et al. (2003) Population based epidemiology of ankle sprains attending accident and emergency units in the West Midlands of England, and a survey of UK practice for severe ankle sprains. Emergency Medicine Journal 20(6), 508-510.
- Cameron, K.L., Owens, B.D. and DeBerardino, T.M., 2010. Incidence of ankle sprains among active-duty members of the United States Armed Services from 1998 through 2006. Journal of athletic training, 45(1), pp.29-38.
- Hubbard, T.J. and Wikstrom, E.A., 2010. Ankle sprain: pathophysiology, predisposing factors, and management strategies. Open access journal of sports medicine, 1, p.115.





Leave a Reply