
Diagnosing & Treating: Rotator cuff related shoulder
Are you struggling with shoulder assessments? Discover how to pinpoint the causes behind rotator cuff related shoulder pain, design personalized treatment plans, and master exercises for pain relief and functionality.
This article will equip your with skills to differentiate between referred pain, stiffness, instability, and soft tissue involvement. Learn techniques from gentle loading to motor control exercises.
Embark on a journey to elevate your shoulder assessment and exercise-based management.
Let’s delve in.
4 Key takeaways of the article
- Tailor exercise programs based on a thorough understanding of the patient’s symptoms, focusing on specific movements to alleviate pain and enhance shoulder function.
- Communicate realistic recovery timelines, addressing both short-term and long-term goals, while recognizing and supporting the emotional aspects of shoulder pain on the patient’s well-being.
- Educate patients about their condition, discussing causes and expected rehabilitation stages, ensuring informed collaboration and realistic expectations throughout the treatment process.
- Implement a holistic treatment plan, addressing underlying factors, and gradually progressing interventions to optimize long-term recovery, minimizing the risk of re-injury.
General rule of thumb for shoulder assessment
It’s crucial for clinicians to figure out the origins of the symptoms so that a patient specific treatment plan can be prescribed.
This involves determining whether the symptoms are:
Referred or Linked to Other Causes: This means checking if the symptoms are coming from somewhere else in the body, such as the neck (cervical), upper back (thoracic) or blood vessels.
Mainly Connected to a Stiff Shoulder: In this case, the focus is on whether the symptoms stem primarily from a shoulder that lacks normal movement. This could be due to conditions like frozen shoulder, osteoarthritis, a shoulder that’s “locked” out of place, or even abnormal growths like osteosarcoma.
Caused by Shoulder Instability: This involves assessing whether the symptoms arise from an unstable shoulder joint, which might be prone to slipping out of place or causing discomfort.
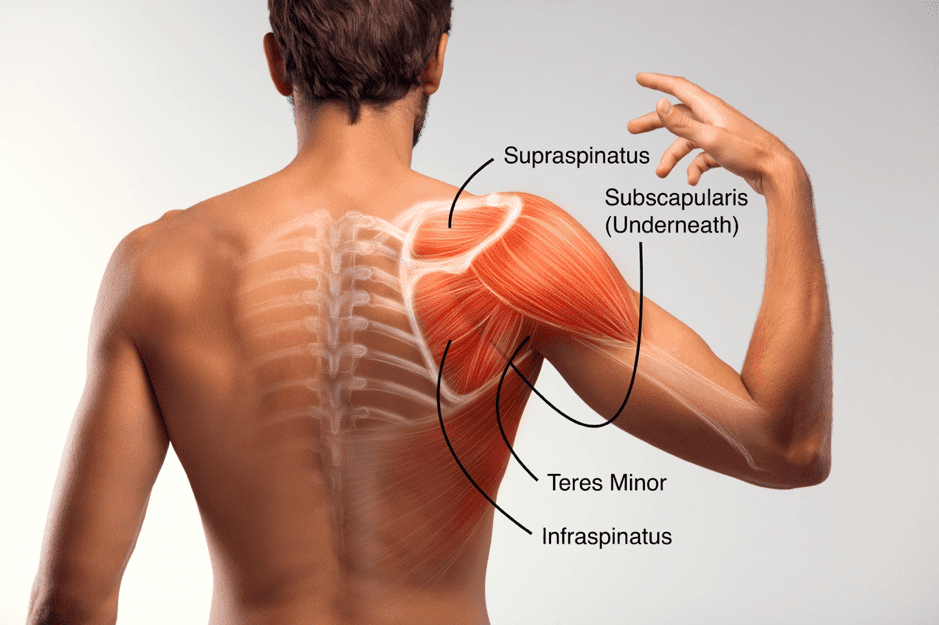
Associated with Soft Tissues (RCRSP): The clinician will also explore whether the symptoms are related to the soft tissues around the shoulder, like the rotator cuff (a group of muscles and tendons), or the bursa (a fluid-filled sac that cushions the joint). Resulting from a
Combination of Factors: Sometimes, symptoms can arise from a mix of the factors mentioned above, making the assessment more complex.
Remember, the assessment process helps clinicians narrow down the potential causes of the symptoms, which is crucial for developing an effective treatment plan.
Special tests for the shoulder
Muscles in the shoulder joint are interconnected:
The way the rotator cuff, the shoulder capsule, and ligaments are woven together actually makes the shoulder more resilient when dealing with heavy loads. This interconnected design helps prevent any single part from failing under pressure.
However, it also means that isolating and testing each individual structure separately becomes quite challenging. The complexity of these interconnections makes it difficult to assess them in isolation.
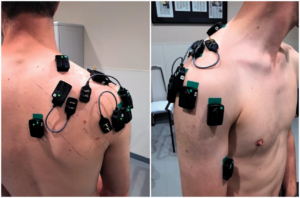
Muscle Activity in Electromyography (EMG):
In electromyography (EMG), a technique used to measure muscle activity, we’ve seen that during tests like the “full can” and “empty can,” which are meant to diagnose issues with the supraspinatus muscle, many other muscles get equally active.
This means that when we’re trying to pinpoint problems with the supraspinatus, a bunch of other muscles join in and contribute to the activity.
Diagnosing RCRSP
Diagnosing RCRSP is a process of elimination, as mentioned above it’s important to determine if the shoulder pain is arising from instability, stiffness, referred from the neck or is it soft tissue related.
The assessment starts with listening to patients:
Things you would be looking to hear to raise suspicion of RCRS:
- History of presenting complaint: (How long have they had it for, is it getting better or worse?)
- Mechanism of injury (have they just bought a house and are painting the rooms? Etc.)
- What positions aggravate the pain? (is it mostly when they lift their hand over head?)
- Is the pain dull or sharp with movement?
- Pain is activity related (better or worse), typically worse reaching overhead or behind the back, with minimal pain at rest except when lying on the affected shoulder
Things that would decreases suspicion of RCRS:
- Is there locking or giving way?
- Do they have pins and needles, numbness or tingling sensation in arm?
- Is the pain consistently the same with or without movement?
- Reproduction of shoulder pain on movement of the neck

Assessing shoulder pain objectively:
Primarily you would do a typical shoulder assessment consisting of:
- ROM of shoulder, cervical spine and thoracic spine
- Strength of the shoulder movements (compare sides)
- Movement under load (external rotation, abduction, flexion)
- Palpation (Humeral head, acromion)
- Shoulder capsule extensibility (compare sides)
- Spurling’s test to determine cervical nerve compression
What you are looking for to raise suspicion:
- There should not be a substantial reduction (>50%) in passive range of motion in any specific direction, notably external rotation.
- Recognisable pain should be triggered through loading or resisted assessments, typically involving abduction and lateral rotation.
- Manipulating the neck’s motion should neither generate nor eliminate shoulder discomfort, and any neurological indications, including upper limb mechanical sensitivity tests, should be absent.

Early management of sensitive shoulder
Build a connection with your patient:
It is essential to recognise that regardless of the specific clinical condition, the first step is to establish a meaningful connection with the individual who is experiencing symptoms. This involves creating an environment where the person feels comfortable expressing their needs and concerns. Empathy plays a crucial role in this process. It’s important to not only comprehend the problem from a clinical perspective but also to acknowledge the emotional and functional impact it has on the patient’s life.
Ask them what they know about their pain:
Patients should be encouraged to openly discuss their understanding of what might be causing their symptoms, their expectations regarding recovery time, their thoughts on potential effective treatments, and their opinions on the treatment plan proposed by the clinician.
Explain the condition, pain pathology and inflammatory processes:
Clinicians, in turn, should provide clear and accurate information about the cause of the issue, the expected course of the problem, and the likely outcomes. It’s important to convey this information in a way that doesn’t use alarming language, avoiding terms that could increase anxiety, such as descriptions of structures impinging or tearing.
Align management expectations:
It’s important to convey to patients that managing tendon-related problems requires the same level of respect and attention as other musculoskeletal issues, like fractures. To illustrate this, consider a person with a fracture in the upper arm or forearm. In such a case, they would be unable to perform certain activities, and compromises would need to be made in their daily routine due to the fracture.
Tendon-related problems often present unique challenges and may require a more extended and complex treatment process compared to fractures. Patients must adhere to appropriate levels of activity and follow the prescribed treatment plan consistently.
Other treatments to consider
Evidence for Shoulder Injection Therapy:
Unfortunately, there is not a substantial amount of strong evidence to strongly support the use of injection therapy for shoulder issues. Some studies have compared injections that provide pain relief alone to injections containing corticosteroids along with pain relief. These studies have shown similar outcomes for up to 6 months after the injection.
In addition, corticosteroids injections have been linked to an increased risk of heart attack (myocardial infarction) and stroke.
Interestingly, this risk can continue to rise even after using these medications for several weeks. Moreover, corticosteroids, a type of anti-inflammatory, have shown negative effects on the health of the rotator cuff tissue.
Considering Analgesic-Only Injections as First-Line:
It’s worth considering analgesic-only injections as a primary choice for injection therapy. One possible reason for this is that both glucocorticoids (which include corticosteroids) and local anesthetics seem to be effective in reducing the number of tenocytes.
Tenocytes are cells associated with tendon issues, and their overgrowth has been linked to tendon problems like tendinopathy.

Role of Ice Wraps in Pain Management:
Anecdotal evidence, while not as robust as scientific studies, suggests that using ice wraps could also play a role in managing pain. Ice wraps might be a helpful tool for controlling discomfort in the shoulder
Key considerations and research findings:
Exercise Program for RCRSP:
A structured exercise plan is the main way to treat RCRSP. However, there’s NO conclusive protocols on how much exercise to do, how often, the right way to do it, how much pain is acceptable, what to do between exercises, and which specific exercises to include.
Be creative and tailor treatment plan to the patients symptoms and motivational levels.
Effects of Exercise:
Exercise has shown both statistical and practical benefits in reducing pain and improving function. However, it doesn’t seem to significantly affect range of motion or increase strength, which is peculiar. Nonetheless, as long as patient feels better it doesn’t necessarily matter what tissue adaptations are made from a rehabilitation point of view.
In addition, combining manual therapy with exercise might make the exercise effects even better (e.g shoulder mobilization).

Home vs. Supervised Exercises:
Doing exercises at home is just as helpful as doing them under supervision.
Research Differences:
One study by Kelly and her team in 2010 found limited evidence supporting the use of exercise. On the other hand, Hanratty and colleagues in 2012 concluded that there’s strong evidence that exercise can reduce pain and make you function better in the short term.
There’s also moderate evidence that exercise can help your mental well-being in the short term and your overall function in the long term.
Why are there differences in the studies?
The differences in what different studies found could be because they looked at different things, used different rules for including or excluding people, used different tools to judge how good the studies were, and used different methods to analyse the results.
Other Factors:
Other things that can affect how well your patients do include their emotions and social factors, how long they have had the problem, their genes, other health issues they have, their lifestyle, and their hormones.
Possible Reason for Not Doing Well:
One reason people might not get the best results is if the treatment doesn’t match exactly what’s going on with them. This has been suggested for other muscle and joint problems too
Exercise based treatment for Irritable and advanced RCRSP
When addressing Rotator Cuff-Related Shoulder Pain, it’s important to understand that providing localized treatment for the shoulder alone may not yield effective results.
A comprehensive approach that considers the broader factors contributing to the condition is necessary for successful management.
Gentle Loading:
Trying exercises that gently engage muscles, like short lever flexion exercises, could be well tolerated. Also, doing shoulder flexion with support from a ball might work, and you can gradually make it more challenging as the patient gets better.
Motor Control & stability:
Focusing on quality of the movement in external rotation as well incorporating low level stability work such as banded bench press to help with rotator cuff control
These exercises should not make the problem worse or give the patient flare ups the following day. Pain level up 4/10 in VAS score is acceptable.
Avoid rushing rehab:
Using high loads, high repetitions and high reps at initial sessions often makes this condition worse. Take it slow and allow the patient to get comfortable and trust the process.
Isometric Exercises:
There’s some evidence that holding a muscle contraction without moving (isometric) in external rotation help control pain. However, there’s no solid proof specifically for the shoulder
Exercise based treatment for non-irritable RCRSP
Similarly cautious approach to loading should be taken at first glance when treating non-irritable RCRSP as in the irritable & advances RCRSP treatment as the condition can switch if too much too soon is done, however it can be progressed faster. The key to tissue adaptation is sufficient load, so as long as the patient doesn’t present with flare ups in the following days then exercises can be progressed.
Guidelines
A consensus done by Littlewood and colleagues named Physiotherapists’ recommendations for examination and treatment of rotator cuff related shoulder pain have concluded on the following factors
Prescribing Active Exercise based on Clinical Assessment:
It is recommended that active exercises should be tailored according to the patient’s clinical assessment rather than solely focusing on their structural pathology. The exercise plan should align with the individual’s specific needs and limitations.
Managing Pain Levels and Timing:
It’s acceptable for patients to experience mild to moderate pain (rated less than 4/10 on the Visual Analog Scale) as a result of the prescribed exercises. However, any pain experienced should resolve within 12 hours after exercising.
Emphasis on Exercise Quality:
The quality of exercise performance is of utmost importance. Patients should engage in exercises while maintaining optimal scapular (shoulder blade) positioning and control. It’s crucial to avoid compensatory movements from the trunk that could hinder the desired outcomes.
Progression Strategy:
Initiate exercises with a focus on simplicity, slowness, and being unloaded. Gradually progress from unloaded exercises to those involving resistance or load, and also from slower to faster movements. The selection of exercises should be limited to a maximum of four, ensuring that each exercise is carefully chosen to suit the patient’s condition.
Individualized Dosing and Progression:
Tailor the dose (intensity, frequency, duration) and progression of exercises to each patient’s unique requirements. Personalize the exercise plan based on the patient’s response to treatment and their progress over time.


Other conditions to be aware of
| Condition | Symptoms |
| Rotator Cuff Tears: | Similar to tendinopathy but may include more significant weakness, sudden pain if tear is traumatic, limited range of motion, clicking or popping sounds during movement. |
| Frozen Shoulder (Adhesive Capsulitis): | Gradual onset of pain and stiffness, restricted shoulder movement in all directions, difficulty reaching behind the back or overhead, pain at night. |
| Labral Tears (SLAP Tears): | Deep, dull shoulder pain, clicking or popping with movement, feeling of instability, pain with lifting or carrying objects |
| Biceps Tendinopathy: | Frontal shoulder pain, worsens with overhead activities or lifting, pain radiating down the upper arm, tenderness in the front of the shoulder. |
| AC Joint Sprain or Arthritis: | Localized pain and tenderness over the AC joint at the top of the shoulder, pain worsens when crossing arms or lifting objects. Glenohumeral (Shoulder) |
| Arthritis | Gradual onset of shoulder pain and stiffness, limited range of motion, pain worsens with movement and weight-bearing |
| Thoracic Outlet Syndrome: | Numbness or tingling in the arm or fingers, pain in the neck, shoulder, and arm, weakness in the hand, worsens with certain arm positions |
| Nerve Entrapment (e.g., Suprascapular Nerve): | Deep ache or burning pain in the shoulder, weakness in specific movements, discomfort may radiate down the arm. Referred Pain (e.g., Cervical Radiculopathy): Symptoms: Neck pain with radiation into the shoulder, arm, or fingers, tingling or numbness along the arm or hand |
| Fractures or Dislocations: | Sudden, severe pain after trauma, visible deformity, limited range of motion, possible swelling or bruising |
Summary of article
Shoulder assessment is crucial for personalized treatment, considering factors like referred pain, stiffness, instability, and soft tissue issues. Special tests for the shoulder are complex due to muscle interconnections, with Electromyography (EMG) tests involving multiple muscles to diagnose Rotator Cuff-Related Shoulder Pain (RCRSP) through a process of elimination.
Acute management involves building rapport, addressing emotional aspects, understanding the patient’s pain perception and expectations, and aligning expectations with a longer treatment duration.
Exercise-based management for RCRSP follows a holistic approach with gentle loading exercises, motor control, stability exercises, and initially avoiding aggressive loading. Guidelines for exercise programs emphasize structured plans, tailored home exercises, and the combination of manual therapy with exercise for enhanced effects.
It is essential to differentiate between various shoulder conditions such as rotator cuff tears, frozen shoulder, labral tears, biceps tendinopathy, AC joint issues, arthritis, nerve entrapment, referred pain, fractures, and dislocations.
Sources
- Hanratty, C.E., McVeigh, J.G., Kerr, D.P., Basford, J.R., Finch, M.B., Pendleton, A. and Sim, J., 2012, December. The effectiveness of physiotherapy exercises in subacromial impingement syndrome: a systematic review and meta-analysis. In Seminars in arthritis and rheumatism(Vol. 42, No. 3, pp. 297-316). WB Saunders.
- Kelly, S.M., Wrightson, P.A. and Meads, C.A., 2010. Clinical outcomes of exercise in the management of subacromial impingement syndrome: a systematic review. Clinical rehabilitation, 24(2), pp.99-109.
- Lewis, J., 2016. Rotator cuff related shoulder pain: assessment, management and uncertainties. Manual therapy, 23, pp.57-68.
- Littlewood, C., Bateman, M., Connor, C., Gibson, J., Horsley, I., Jaggi, A., Jones, V., Meakins, A. and Scott, M., 2019. Physiotherapists’ recommendations for examination and treatment of rotator cuff related shoulder pain: A consensus exercise. Physiotherapy Practice and Research, 40(2), pp.87-94.





Leave a Reply