
Treating patellofemoral pain with confidence
Patellofemoral pain, this common knee condition can be debilitating, but there’s hope. In this article, we will explore the complexities of diagnosing and treating PFP, offering insights into its causes, assessment methods, and effective management strategies.
Whether you’re a clinician seeking diagnostic guidance or an individual experiencing PFP, our comprehensive overview will provide the information you need to understand, address, and ultimately conquer this challenging condition.
Read on to discover the key assessment tests, treatment modalities, and return-to-sport criteria that can make a significant difference in the lives of those affected by Patellofemoral Pain.
5 Key takeaways
- Diagnosing Patellofemoral Pain involves comprehensive subjective and objective assessments, often ruling out other knee conditions before diagnosing PFP
- Key diagnostic tests for PFP is the squat test
- Effective PFP management includes personalised exercise-based therapy, patient education, activity modification & stretching (determined by muscle tone limitations)
- Medication and taping therapies may be used alongside exercise-based treatments, but their efficacy varies, and taping should complement exercise.
- Athletes should meet specific criteria, including absence of swelling, pain-free movements, adequate strength, flexibility, normal gait biomechanics, core stability, and confidence before returning to sports after PFP.
Subjective Assessment of PFPS
Patellofemoral Pain is a common ailment among athletes, characterised by pain around the kneecap that can worsen during weight-bearing activities.
Diagnosing and treating PFP can be challenging, requiring a comprehensive evaluation.
Understanding Chronicity and Training History
Diagnosing PFP involves an extensive subjective examination that probes into the athletes activities before symptom appearance as well as aggravating and easing factors during.
In many cases, PFPS is attributed to overuse, making it crucial to investigate recent changes in an athlete’s sporting activities.
This includes alterations in training frequency, duration, and intensity. Errors in the training program, such as rapidly increasing exercise intensity, inadequate recovery time, and extreme hill workouts, should be considered.
PFP can sometimes present as an acute re-exacerbation of a chronic condition.
Additionally, factors such as :
- The use of inappropriate or excessively worn footwear
- Recent heavy resistance training and conditioning activities (especially squats and lunges)
- Running on altered surfaces or hills.
Traumatic knee injuries, patellar subluxation, dislocation, or surgeries should also be noted, as they may directly damage the articular cartilage or change forces across the patellofemoral joint, leading to PFP.
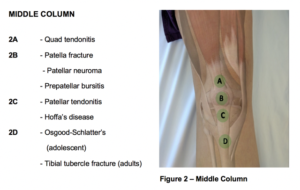
When examining the causes of Patellofemoral Pain, it is crucial to rule out other potential factors, including intra-articular abnormalities, plica syndromes, Osgood-Schlatter disease and neuromas.
Objective Assessment of PFPS
Whilst you can diagnose PFP with a subjective assessment alone, objective test can help cement the diagnosis and pinpoint areas to work on during rehab.
However, it’s crucial to note that there is no definitive clinical test to diagnose PFP. Various tests have been proposed, but common tests lack sensitivity.
This makes PFP a diagnosis of exclusion, often identified after ruling out other knee conditions, such as tibiofemoral osteoarthritis, plica syndrome, or other similar issues.
Key Tests for PFPS Diagnosis
Squat:
According to the recent consensus statement from the Fourth International Patellofemoral Pain Research Retreat, anterior knee pain elicited during a squatting is the best available test, and patellofemoral pain is evident in 80% of people who are positive on this test
Vastus Medialis Coordination Test:
This test evaluates coordination during knee extension and can indicate limitations in vastus medialis muscle coordination
Description: While the patient lies supine, the examiner positions their fist beneath the patient’s knee, instructing them to slowly extend their knee without exerting pressure or lifting away from the examiner’s hand.
Full extension should be achieved.
A positive test indicates a lack of coordinated full extension, where the patient faces difficulty in achieving smooth extension and may rely on hip extensors or flexors for the extension, suggesting potential dysfunction of the vastus medialis obliquus muscle.

Patellar Apprehension Test:
Involving a lateral patellar glide, this test is used to reproduce patient pain or apprehension.
Description: The patellar apprehension test, sometimes called the Fairbanks apprehension test, is conducted with the patient lying supine and relaxed. During this test, the examiner gently pushes the patient’s patella laterally to create a lateral patellar glide. Starting with the knee flexed at 30°, the examiner holds the leg at the ankle/heel with one hand and performs a gradual flexion in the knee and hip while maintaining the lateral glide .
A positive outcome is observed when the test reproduces the patient’s pain or elicits apprehension

Eccentric Step Test:
In this test, patients step down from a platform to assess knee pain during the test.
Description: In the eccentric step test, patients perform the assessment without footwear. The step’s height is typically set at 15 cm or approximately 50% of the tibia’s length
During the test, each patient is instructed to stand on the step, place their hands on their hips, and gently step down as slowly and smoothly as possible. The patient should maintain their hands on their hips throughout the test. After completing the test with one leg, it is repeated with the other leg without any warm-up or practice attempts.
A positive result on the eccentric step test is indicated when the patient experiences knee pain during the test have own pics

Single Leg Squat:
This test assesses dynamic hip and quadriceps strength and reveals compensatory movements in patients with PFPS.
Explanation: The single-leg squat assesses dynamic hip and quadriceps strength, placing greater mechanical demands compared to a bilateral squat, possibly leading to compensatory movements like knee valgus. These challenges could result from the smaller base of support and the increased need for dynamic control in multiple planes during the single-limb squat.
Patients with PFP, in comparison to controls, exhibited increased ipsilateral (same side) trunk lean, contralateral (opposite side) pelvic drop, hip adduction, and knee abduction when performing a single-leg squat have own pics
Tenderness & palpation:
Tenderness on palpation of the patellar edges is a test with limited evidence as PFP is evident in 71%–75% of people with this finding.
Sign up to the free newsletter and get breakdown of latest sports medicine research: Link
Early management of patellofemoral pain
Patellofemoral pain is a complex and challenging musculoskeletal condition characterised by its widespread prevalence, chronic nature, and the substantial burden it imposes on individuals. Timely and effective intervention is pivotal in mitigating the long-term implications.
However, the absence of well-established treatment guidelines complicates the planning of treatment. While sports medicine experts suggest various approaches, the lack of standardised protocols underscores the intricate and multifaceted nature of this condition.
Personalised Treatment Approach:
To address PFP effectively, there is no universal solution. Instead, a tailored clinical approach is essential. Practitioners must systematically assess and manage a variety of risk factors, encompassing localised knee issues, proximal factors involving the trunk and hip, and distal factors relating to the foot and ankle.
Addressing low hanging fruit such as ROM deficits and/or biomechanical movement patterns (i.e knee valgus, un-equal weight distribution etc.) through functional tasks can be good starting points
Patient Education:
Furthermore, educating patients plays a significant role in the recovery process, indirectly enhancing exercise adherence. This involves providing patients with comprehensive information about the clinical course and establishing clear expectations. Emphasising potential consequences if the treatment plan is not followed can motivate patients to adhere.
Additionally, offering informative leaflets can be a powerful tool for clinicians, equipping patients with knowledge about their condition and its management, thereby fostering active participation in their own care.

Activity Modification:
In the case of athletes with PFP, the importance of relative rest and activity modification cannot be overstated. When overuse is a prominent factor in PFP, the positive impact of rest becomes evident.
In acute injuries, allowing affected tissues to heal through relative rest can reduce symptoms. However, in chronic cases, managing daily activities that may exacerbate pain can be challenging, highlighting the crucial role of patient education in guiding individuals to avoid excessive joint loading, a central aspect of successful PFP management.
Other treatment to consider
Foot Orthosis:
The effectiveness of foot orthosis in patellofemoral pain treatment remains a topic of debate. According to a consensus statement, foot orthosis may provide short-term pain relief. A systematic review found limited evidence for prefabricated foot orthosis, with better results observed when combined with physiotherapy.
It’s important to note that individual responses to foot orthosis treatment vary, and specific clinical characteristics, such as midfoot mobility and ankle dorsiflexion, can help predict the success of this intervention. Highlighting the fact that there’s no size that fits all. Prescribe treatment to patients determined on their clinical presentation, rather the conditions that they come in with.

Neuromuscular Electrical Stimulation (NMES):
NMES involves inducing muscle contractions using electrical impulses. Some proponents argue that NMES can be integrated into cost-effective home-based therapy regimens, but it hasn’t proven more effective than formal supervised physical therapy when used in isolation.
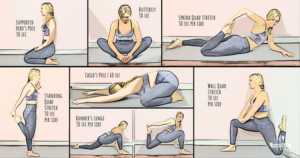
Stretching:
Stretching various muscle groups, including the hamstrings, quadriceps, iliopsoas, gastrocnemius, and iliotibial band, has been explored for PFP. It’s theorised that tightness in these muscle groups may affect patellofemoral joint forces.
Stretching, either alone or combined with strengthening exercises, can alleviate symptoms in up to 60% of patients. Proprioceptive neuromuscular facilitation stretching techniques, like the contract-relax method, may offer advantages over traditional static or ballistic stretching exercises.
Again, keep in mind that this approach may be most beneficial for patients that have shortened muscles (determined by objective examination) and thus can be an excellent option for majority, and a time waster for a few.
Pharmacotherapy:
Medication including simple analgesics like aspirin and NSAID’s (ibuprofen), is sometimes used for managing PFP. However, evidence for the efficacy of these medications, particularly NSAIDs, is limited.
While short courses of NSAIDs may be considered when other treatments have failed, their use is debated due to the absence of inflammation in many PFP cases and concerns about potential adverse effects on muscle and tendon healing responses.
Role of taping
Therapies like taping, proprioceptive training and shoe inserts can be most effective when used in conjunction with traditional exercise therapy. However, they tend to be less effective when implemented on their own.
Various taping methods are available, such as:
- McConnell taping
- Infrapatellar taping
- Kinesiotaping
- Other custom taping approaches.
McConnell tape is a rigid adhesive designed for structural support, while Kinesiology tape is more flexible, allowing gentle muscle stretching without restricting motion.
McConnell taping aims to reposition the patella within the femoral trochlea, theoretically reducing pain associated with PFP and enhancing quadriceps and patellofemoral movements.
Research suggests that knee taping, when combined with exercise, can offer better pain reduction compared to exercise alone. However, knee taping on its own may not effectively control pain. Rigid taping (like McConnell taping) is often preferred as it creates space between the patella and the trochlea.
Several studies have shown the efficacy of patellar taping and bracing in reducing pain and improving postural and functional control. Taping for the patellofemoral joint aims to mechanically adjust the patella’s position and enhance its tracking within the trochlear groove.
Both traditional nonelastic tape and modern elastic Kinesio Tape have been used for this purpose, with varying degrees of success. However, the timing of tape application and its clinical significance remain subjects of debate.

Exercise based management for patellofemoral pain
Physical therapy is widely accepted as the initial and effective approach to managing patellofemoral pain. Systematic reviews and meta-analyses consistently demonstrate the positive impact of exercise interventions in reducing pain and improving function for PFP patients.
Exercise therapy is also cost-effective and recommended, especially for young adults. The mode of exercise therapy may vary, but strength exercises, including knee extension, squats, and more, are generally beneficial.
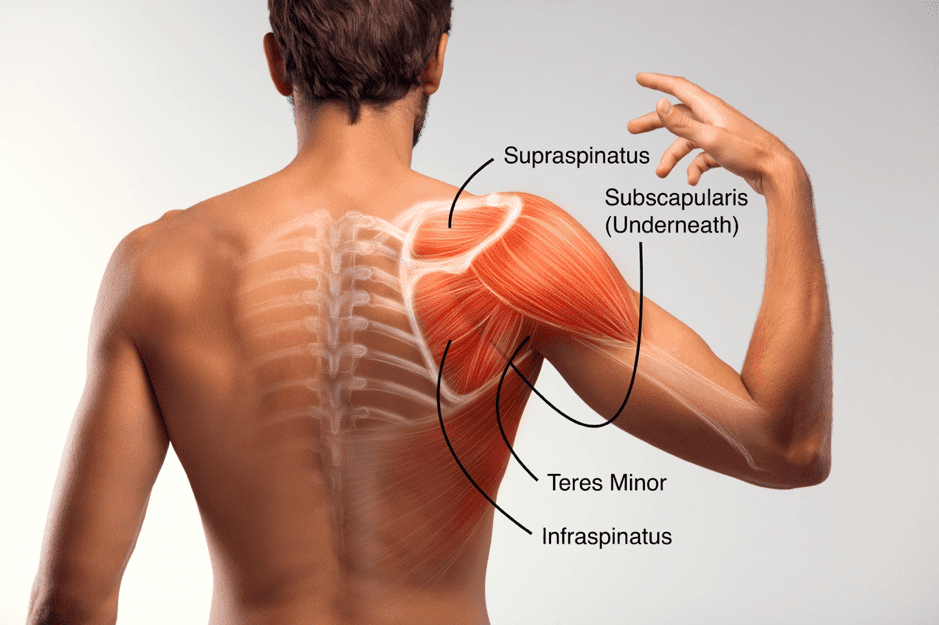
It’s crucial to focus on pain-free exercises and consider both weight-bearing and non-weight-bearing activities at specific knee flexion angles. Emphasizing the vastus medialis oblique, hip abductors, external rotators, and core stability is essential.
Areas of focus:
- Ankle proprioception and balance
- Knee
- Hip
- Abdominals/trunk/core
Exercise Recommendations
- Split squat | Hamstring bridge | Side plank | Y-balance
- Step down | Single leg RDL’s | Hip thrust | Un-even surface balance with ball catching (a little more fun)
Open vs. Closed Chain Exercises:
Closed chain exercises, which mimic weight-bearing activities, are preferred over open chain exercises like leg extensions, which can worsen symptoms. Studies show that both open and closed chain exercises result in significant functional improvements in PFP patients.

Strengthening:
Quadriceps strengthening is essential in PFP management, but hip and abdominal muscle strengthening is equally critical. Research indicates that programs targeting these muscle groups provide pain relief and improved function. Combining quadriceps strengthening with hip abductor and abdominal exercises is particularly beneficial.
Flexibility:
Tissue tightness in various muscle groups, including the quadriceps, hamstrings, iliotibial band, and gastrocnemius, can contribute to patellofemoral pain. Flexibility training is recommended as a supplement to strengthening in physical therapy. However, it’s important to note that the effectiveness of flexibility training can vary based on the individual’s muscle tone.
Return to sport with PFP
Elite athletes, in particular, often face the pressure of returning to competition swiftly, especially when significant events are on the horizon. Whilst it may be unrealistic to have all these factors completely absent in the real world scenario, It’s advisable to have as many of them under control and close to ‘normal’ as possible.
Athlete checklist for sports participation clearance:
Absence of Swelling:
The injured area should exhibit no swelling, indicating that the inflammation has subsided.
Pain-Free Movements:
The athlete should experience no pain when squatting or when navigating stairs, whether ascending or descending.
Quadriceps Strength:
Adequate quadriceps strength is essential compared to opposite side (10% difference is acceptable). You can use dynameter to measure accurately
Hamstring Flexibility:
80 degree hamstring range through straight leg raise is advisable
Normal Gait Biomechanics:
The athlete’s walking pattern should demonstrate normal biomechanics, without any noticeable limping, weight shifting or knee position
Core Stability:
Adequate core stability is important to support the body’s movements and overall stability. Whilst flawed, you can measure this objectively by asking the patient to do a plank. A good number to achieve is 2minute hold, which indicates adequate core endurance.
Functional Tests:
Pain free or VAS score of 1/2 in challenging functional tests, such as vertical jumping, lunges, step-down exercises, single-leg presses, and balance is required.
Athlete Confidence:
Importantly, the athlete should personally feel ready and confident in the healing of their injured knee.
Other conditions to be aware of

Summary of article
- Patellofemoral Pain (PFP) is a common issue among athletes, characterized by knee pain during weight-bearing activities.
- Diagnosing and treating PFP requires a comprehensive assessment, with both subjective and objective elements.
- Subjective assessment involves examining the athlete’s training history, identifying overuse factors, and potential acute exacerbations of chronic conditions.
- Objective assessments help confirm PFP and guide treatment but lack a definitive clinical test.
- Key objective tests include the squat, vastus medialis coordination test, patellar apprehension test, eccentric step test, single-leg squat, and tenderness and palpation of patellar edges.
- Effective PFP management involves personalized treatment, patient education, activity modification, foot orthosis, neuromuscular electrical stimulation, stretching, and pharmacotherapy.
- Taping, like McConnell taping, is more effective when combined with exercise therapy.
- Exercise-based management is widely recommended, with a focus on strength exercises, closed chain exercises, and flexibility training if necessary.
- Athletes can return to sports when specific criteria are met, including the absence of swelling, pain-free movements, good quadriceps strength, normal gait biomechanics, proper core stability, success in functional tests, and athlete confidence.
Sources
- Barton, C.J., Munteanu, S.E., Menz, H.B. and Crossley, K.M., 2010. The efficacy of foot orthoses in the treatment of individuals with patellofemoral pain syndrome: a systematic review. Sports Medicine, 40, pp.377-395.
- Farzin Halabchi, Maryam Abolhasani, Maryam Mirshahi & Zahra Alizadeh (2017) Patellofemoral pain in athletes: clinical perspectives, Open Access Journal of Sports Medicine
- Logan, C.A., Bhashyam, A.R., Tisosky, A.J., Haber, D.B., Jorgensen, A., Roy, A. and Provencher, M.T., 2017. Systematic review of the effect of taping techniques on patellofemoral pain syndrome. Sports health, 9(5), pp.456-461.
- Rothermich, M.A., Glaviano, N.R., Li, J. and Hart, J.M., 2015. Patellofemoral pain: epidemiology, pathophysiology, and treatment options. Clinics in sports medicine, 34(2), pp.313-327.





Leave a Reply