
Physiotherapist’s Toolkit for Diagnosing Plantar Fasciitis
As a physiotherapist, have you ever encountered patients complaining of heel pain? It’s a common condition that affects many individuals, and if not treated promptly, it can cause significant discomfort and hinder their daily activities. Plantar heel pain is a prevalent musculoskeletal disorder, accounting for up to 15% of foot-related complaints seen in clinical practice. It is commonly associated with a variety of underlying causes, including plantar fasciitis, calcaneal stress fracture, and Achilles tendinopathy, among others.
To effectively manage and treat plantar heel pain, it is essential to have a good understanding of its clinical presentation, possible risk factors, and clinical course. This knowledge will help in developing an appropriate management plan for each patient based on their unique needs and goals.
In this article, we will provide you with an overview of the causes, symptoms, clinical presentation, clinical course, and risk factors associated with plantar heel pain. We aim to equip you with the knowledge and skills required to diagnose, manage, and treat this condition effectively, ultimately improving the quality of care you provide to your patients.
Click here to Learn how to treat plantar heel pain
5 Key Takeaways
- Plantar heel pain, or plantar fasciitis, is a common condition causing pain in the bottom of the foot, particularly the heel, often aggravated by activities like walking and running.
- It accounts for a significant portion of foot symptoms requiring professional care, affecting around 11-15% of adults, and is prevalent among runners and military personnel.
- The plantar fascia, a fibrous structure that maintains the arch of the foot, plays a crucial role in this condition.
- Contributing factors include overuse, abnormal foot mechanics, a shortened Achilles tendon, and high-impact activities.
- Plantar heel pain typically presents as sharp pain in the heel, often worse in the morning, and can be diagnosed clinically, with imaging sometimes used to confirm or rule out other conditions.
What is plantar heel pain?
Plantar heel pain, also known as plantar fasciitis, is a condition that affects the bottom of the foot, specifically at or near the calcaneal attachment. It is a common condition that can cause pain and discomfort, especially with activities such as walking or running.

Fun Facts – Plantar Heel Pain
- Plantar fasciitis is estimated to be the most common cause of pain in the inferior heel, accounting for approximately 11 to 15 percent of all foot symptoms that require professional care among adults.
- Plantar heel pain has been reported to account for about 10% of injuries that occur in connection with running. This is due to the repetitive impact and load placed on the plantar fascia during running.
- Plantar heel pain is also common among military personnel. The physical demands of military training such as, prolonged standing, running, and wearing heavy boots put accumulative stress on the plantar fascia.
- Plantar heel pain tends to peak in people between the ages of 40 and 60 in the general population. Reduced flexibility and age-related changes on the plantar fascia structure, may contribute to the higher prevalence of plantar heel pain.
- Plantar heel pain affects a significant portion of the population, with estimates ranging from 7% to 10%. It is a relatively common condition that can cause discomfort and pain in the heel, impacting daily activities and quality of life for many individuals.
Anatomy of plantar fascia
Origin:
The plantar fascia originates from the medial tubercle of the calcaneus, which is a bony prominence on the medial side of the heel bone.
Insertion:
The plantar fascia fans out and inserts into the base of the metatarsal bones. It attaches to the plantar plates, which are fibrous structures that connect the metatarsal heads to the proximal phalanges.
Fibres:
The plantar fascia is composed of tightly arranged collagen fibres, which provide strength and stability to the foot arch. The fibres are oriented in a longitudinal direction along the length of the plantar fascia, allowing it to resist tension and absorb shock during weight-bearing.
Function:
The plantar fascia plays a crucial role in maintaining the arch of the foot and providing stability during weight-bearing activities, such as walking, running, and jumping. It acts like a bowstring, absorbing and storing energy as the foot flattens during load and then releasing that energy during push-off to propel the foot forward.
Blood supply:
The plantar fascia has a limited blood supply, with most of its nutrition coming from adjacent tissues. This is one of the reasons why plantar heel pain can be tricky to rehabilitate.

What causes plantar heel pain?
The cause of plantar heel pain is poorly understood and is probably multifactorial. Weakness or imbalances in muscles such tibialis anterior, tibialis posterior & peroneus longus can potentially affect the overall function and stability of the foot, which may contribute to altered foot mechanics and increase stress on the plantar fascia, indirectly leading to plantar heel pain.
However, whilst they play a role in supporting the arch of the foot, weakness in these muscles alone is not typically a primary cause of plantar heel pain.
Something to think about:
Overuse or excessive activity: Repetitive stress on the plantar fascia without adequate rest or sudden increase in activity such as running, jumping, or prolonged standing, especially on hard surfaces, can place load that the tissue is not yet able to withstand.
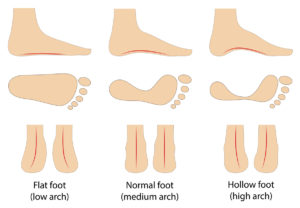
Foot mechanics: Abnormal foot mechanics, such as flat feet (overpronation) or high arches (supination), can alter the biomechanics of the foot and increase the strain on the plantar fascia.
Shortened Achilles tendon: A shortened Achilles tendon can alter the normal mechanics of the foot and ankle. This can increase the load on the plantar fascia which ultimately leads to plantar heel pain.
Epidemiology | Frequency & Pattern
The epidemiology of plantar heel pain is the study of the occurrence, distribution, and determinants of this condition in populations. Epidemiological data on plantar heel pain is limited, as it is often a self-limiting condition that does not always require medical attention. However, based on available studies and clinical observations the prevalence of plantar heel pain is as follows;
Prevalence: The prevalence varies depending on the population studied and the criteria used for diagnosis. Studies have reported a wide range of prevalence rates, with estimates ranging from 4.5% to 10% in the general population. It is more commonly reported in middle-aged individuals, but it can occur in people of all ages.
The clinical presentation
Plantar heel pain typically presents as pain and discomfort in the heel, particularly with weight-bearing activities like walking or running. The pain is often sharp and may be more severe in the morning or after prolonged periods of rest. It’s important to know key points to listen to when your client is speaking for you to comfortably diagnose plantar heel pain.
Subjective information may include;
- Reports of gradual onset of pain at the heel (Usually calcaneal insertion) that is most commonly worse with their first steps in the morning or after a period of in-activity.
- Clients may describe limping with the heel off the ground (on their top-toes).
- The pain tends to lessen with gradually increased activity but worsens toward the end of the day with increased duration of weight-bearing.
- Numbness, pins n’ needles and/or tingling is very uncommon.
Patients may report that before the onset of their symptoms:
- They increased the amount or intensity of their regular walking or running regimen.
- Exercised on different surfaces (Concrete, sand).
- Used different footwear.
Objectively you may find;
- Stiffness or tightness in the calf muscles
- Reduced range of motion in the ankle joint
- Tenderness at the bottom of the heel upon palpation
How long does plantar fasciitis last?
In many cases, patients can expect significant improvement and resolution of symptoms within 10 months of conservative management, with success rates reported to be over 80%. Factors such as quality rehab, nutrition, and lifestyle changes can play a role in speeding up the recovery.
- Tailored rehabilitation, which may include guided exercise programs can help improve foot and lower leg strength, flexibility, and tissue load tolerance.
- Adequate nutrition, including a balanced diet with essential nutrients, can support tissue healing and reduce inflammation, which can contribute to faster recovery.
- Lifestyle changes such as maintaining a healthy body weight, avoiding activities that exacerbate symptoms to an un-bearable level, and modifying footwear or daily activities as needed can also positively impact recovery from plantar heel pain.
Sign up to our free newsletter here
The role of Imaging
Imaging can play a supportive role in the diagnosis of plantar heels pain , but it’s definitely not always necessary to make a clinical diagnosis. Plantar heel pain is typically diagnosed based on the patient’s clinical history, symptoms, and physical examination findings.
However, imaging studies may be used in certain cases to confirm the diagnosis or rule out other conditions that may present with similar symptoms. The following imaging modalities are commonly used in the diagnosis of plantar heel pain:
- X-ray: X-rays are often the initial imaging study performed for evaluating plantar heel pain. X-rays can help rule out other conditions such as fractures, tumours, or arthritis that may present with similar symptoms.
- Ultrasound: Ultrasound can provide detailed images of the plantar fascia, allowing for visualization of its thickness, integrity, and any signs of inflammation or degeneration.
- Magnetic Resonance Imaging (MRI): Similarly to ultrasound MRI can provide images that can help visualize the anatomy of the plantar fascia, assess its integrity, and identify any signs of inflammation or degeneration. MRI provides higher resolution than ultrasounds, thus giving more information. It’s a more advanced imaging modality and is typically reserved for cases where other imaging studies are inconclusive or when there is suspicion of other conditions, such as tumours or nerve impingements.
Risk factors for developing plantar fasciitis
Understanding the risk factors associated with plantar heel pain can help determine clients who may be at higher risk for developing this condition. Identifying and addressing these factors early in the treatment programme can help prevent or reduce the intensity of the symptoms.
Having high arched foot
Individuals with high-arched feet, also known as pes cavus, may have altered biomechanics of the foot. Leading to decreased shock absorption and increased pressure on the heel and forefoot, which may overload and irritate the tissue.
Obesity
Excess body weight puts increased load on the plantar fascia, as it has to bear more load during weight-bearing activities.
Occupations that require prolonged standing/walking
Jobs that require prolonged standing or walking, such as retail, healthcare, or manufacturing, can result in repetitive stress on the plantar fascia.
Excessive pronation of foot
Pronation is the natural inward rolling of the foot during walking or running. However, excessive pronation, can cause altered foot mechanics and increase stress on the plantar fascia.
Reduced ankle dorsiflexion
Ankle dorsiflexion is the movement that allows the foot to bend upward toward the shin. Reduced ankle dorsiflexion, or limited flexibility in this movement, can alter foot mechanics and cause compensatory changes in gait, potentially increasing stress on the plantar fascia.
High prevalence in runners
Runners, especially those who engage in repetitive high-impact activities such as long-distance running or sprinting, are at an increased risk of developing plantar heel pain due to the repetitive stress and strain on the plantar fascia during running
Sedentary lifestyle
Inactivity, or a sedentary lifestyle, is not typically considered a direct risk factor for developing plantar fasciitis. However, having limited exercise deconditions the tissues and thus after sudden increase in activity, such as going hiking, starting a job that that requires prolonged walking/standing. The tissues are not able to withstand the load that they are given. It’s important to strike a balance between appropriate physical activity and rest, and to gradually increase activity levels to minimize the risk of developing plantar heel pain.

Summary of article
- Plantar heel pain, or plantar fasciitis, affects the bottom of the foot near the calcaneal attachment.
- It is a prevalent condition, constituting about 11 to 15 percent of foot symptoms requiring professional care in adults.
- Multiple factors contribute to plantar heel pain, including overuse, abnormal foot mechanics, and a shortened Achilles tendon.
- Commonly reported in middle-aged individuals and accounts for approximately 10% of running-related injuries.
- Clinical presentation involves gradual onset of heel pain, often most severe with the first steps in the morning or after inactivity
Sources
- Buchbinder, R., 2004. Plantar fasciitis. New England Journal of Medicine, 350(21), pp.2159-2166.
- Davis, P.F., Severud, E. and Baxter, D.E., 1994. Painful heel syndrome: results of nonoperative treatment. Foot & Ankle International, 15(10), pp.531-535.
- Lopes, A.D., Hespanhol, L.C., Yeung, S.S. and Costa, L.O.P., 2012. What are the main running-related musculoskeletal injuries? A systematic review. Sports medicine, 42, pp.891-905.






Leave a Reply