A Guide to Calf Strain: Assessment & Effective Recovery Strategies
Muscle injuries are a common occurrence in sports and in the general public. The management of these injuries is essential for optimizing recovery and return to sport. As physiotherapist, we need to understand the principles of assessment, acute management, exercise-based management, and return to sport criteria to effectively manage these injuries.
In this article, we’ll explore these four key components in detail, discussing the importance of each stage and how they contribute to the overall management of musculoskeletal injuries. We’ll also examine the latest evidence-based approaches to injury management and highlight the best practices for promoting safe and effective rehabilitation.
By understanding these areas you will be able to develop a well-rounded approach to managing calf strains. It will help to optimize patient outcomes, reduce the risk of re-injury, and promote safe and effective return to sport.
Lets have a look!
5 key Takeaways
- Assess calf muscle injuries by performing palpation to identify tender spots, active and passive range of motion tests, and strength testing to determine muscle damage and treatment plans.
- In the acute phase of calf strain, rest, elevation, and careful management of NSAIDs are essential, and compression bandages may speed up recovery.
- Rehabilitation in the subacute phase includes passive and active stretches (if reduced ROM), soft-tissue techniques, and muscle strengthening exercises.
- Exercise-based management, including progressive overload with balance/proprioception & calf strength, helps promote tissue repair, muscle strength, and range of motion.
- Return to play strategies are crucial, involving specific tests and gradual reintroduction of physical activity to prevent re-injury, with six recommendations for designing a program provided.
Assessing calf strains
Assessing the extent of muscle injury or specifically calf complex injury is an essential component of a physiotherapist’s job. After the subjective assessment where you determine the when and the how.
The next step is to perform an objective assessment.
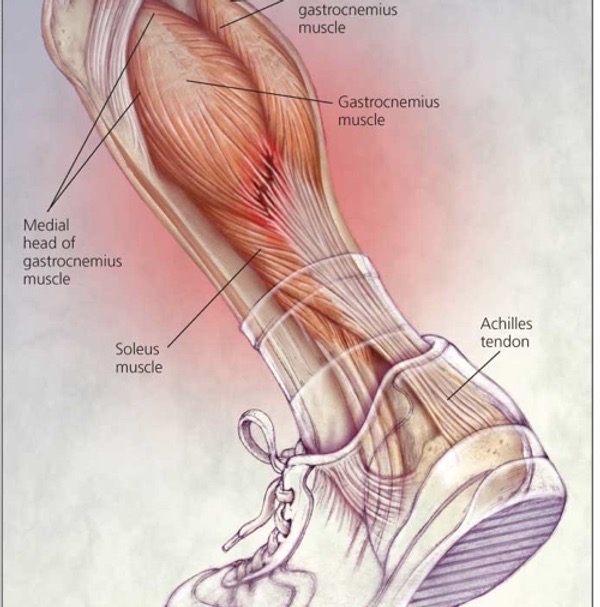
1– Palpation is often the first step in assessing a calf strain as it helps to identify any tender spots, which can be an indicator of muscle damage. It’s important to note that tenderness in the medial gastrocnemius belly can be normal and is common even in uninjured athletes. A crucial step in assessing the calf strain is to distinguish which muscle is affected, as the treatment protocols are different. Tenderness in the medial gastrocnemius belly or the musculotendinous junction indicates gastrocnemius strain, whereas tenderness distal and lateral to the gastrocnemius implicates the soleus
2 – Active ROM of the ankle and knee are used to determine the extent of the injury and whether the client is able to actively move its joints without restrictions (guarding due to pain & swelling) compared to un-affected leg. It assesses the strength, flexibility, and coordination of the muscles and the nervous system that control joint movement.
3 – Passive ROM assesses the integrity of the joint capsule, ligaments, tendons, and other structures surrounding the joint. Passive ROM testing can also help identify any restrictions or limitations in joint movement due to injury, inflammation, or other conditions
Note.
In general, active ROM testing is used to assess the functional ability of a person to move their joint in daily activities, while passive ROM testing is used to assess the structural integrity of the joint and detect any abnormal or restricted movements.
4– Strength testing can be used to evaluate the extent of muscle damage and to determine the ability of the muscle to generate force. This is important in determining the appropriate treatment and rehabilitation plan for the patient. You can use handheld dynameter to have a more accurate reading or oxford grading scale if you don’t have access to special equipment.
If a patient has a severe calf strain, they may require a longer period of rest and rehabilitation before returning to their normal activities. Strength testing can also help to identify any muscle imbalances or weaknesses that may have contributed to the calf strain in the first place. Addressing these imbalances through targeted strengthening exercises can help to prevent future injuries.
Additionally, strength testing can be used to track the progress of recovery.

How to manage calf strains early?
Acute — In the acute phase, treatment is designed to protect the injured tissue by reducing activity, managing pain, and preventing haemorrhage or other complications.
- In the first 24 to 72 hours, activities should be limited to allow the injured leg to be rested in an elevated position and NSAID use should be carefully managed (if any) due to their ability to impede the inflammatory processes. These processes are essential for optimal healing and recovery
- High compression bandages that exert 20 to 30 mm Hg of pressure have been recommended in published reports, and some evidence has suggested that compression bandage use can improve recovery by up to 7 days
- Massage & heat are contraindications due to increased risk of haemorrhage
Sub-acute — In the subacute phase, the body repairs the soft-tissue damage and forms scar tissue.
- The goal of treatment is to improve mobility, prevent muscle atrophy or contracture, and facilitate tissue regeneration in order to optimize functional recovery
- Rehabilitation includes passive and active stretches, soft-tissue techniques, muscle strengthening, and proprioception exercises for 2 weeks.
- Stretching elongates the intramuscular scar tissue in preparation for strengthening exercises (dependent on pain & severity of strain).
- As range of motion improves and pain subsides, strength training can progressively incorporate isometric, isotonic, and dynamic exercises as tolerated without pain.
Exercise based management
As a clinician, you are well aware of the evidence supporting the use of exercise-based rehabilitation after a muscle strain. Exercise can promote the release of growth factors and cytokines, which can aid in tissue repair and regeneration. By increasing blood flow to the affected area, exercise can deliver essential nutrients and oxygen to the muscles, which can stimulate the healing process.
Moreover, specific exercises can help to restore muscle strength, range of motion, and flexibility, which are crucial for functional recovery. Exercise can also prevent the development of scar tissue and muscle imbalances, which can lead to long-term complications.
By implementing a structured exercise program based on the principles of progressive overload, specificity, and individualization, you can help your patients to safely and effectively recover from their calf strain and improve their overall muscle function.
Here are a few exercises to try.
- Double leg STANDING (Gastro) heel raises (3 sets / 25 reps)
- Double leg STANDING KNEE BENT (Soleus) heel raises (3 sets / 25 reps)
- Horizontal & lateral heel raises to mimic running and sprinting (3 sets / 15 reps)
- Single leg RDL —> Knee drive RDL (3 sets / 30-60 sec)
- Body weight/loaded squats (3 sets/ 8-12 reps)
List of equipment used:
- Kettle bell(s)
- Step
Other treatment options
Whilst exercise based management is the gold standard for muscle strains there are a few options out there that can be beneficial in a clinical and elite sport setting. Let have a look.
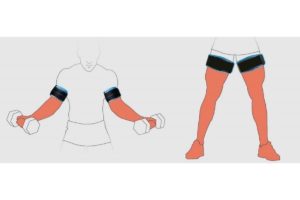
Blood flow restriction training (BFRT)
is a form of light resistance training that involves using a restriction band proximally on the extremity to occlude venous blood outflow while maintaining arterial blood inflow.
- Light resistance training applies mechanical stress to the muscles, and the use of a restriction band induces tissue hypoxia, which stimulates anaerobic metabolism
- Studies have shown that BFRT can increase muscle strength, hypertrophy, and angiogenesis compared to unrestricted light resistance training. However, less muscle is recruited compared to unrestricted heavy resistance training.
- The biological mechanism underlying BFRT is not yet fully understood. However, the combination of mechanical and metabolic stress is thought to activate cellular signalling pathways that lead to protein synthesis, fast-twitch muscle fibre recruitment, and stimulation of myogenic stem cells.
- BFRT may be useful as a progressive rehabilitation method to promote the regeneration and healing of muscle, especially in situations where heavy resistance training is contraindicated in the early stages of recovery.
Deep water running
Is a form of rehabilitation exercise that involves running in a pool where the feet do not touch the bottom. The individual wears a flotation device to keep them buoyant and can perform running movements without any impact on the lower limbs. This type of exercise is often used in lower limb rehabilitation as it allows individuals to engage in weight-bearing exercise without putting stress on their joints or muscles.
Lower body positive pressure (LBPP)
Is a therapy is similar to deep water running but instead of water it involves creating a pressurised environment around the legs while the individual is walking or exercising. This is typically achieved by placing the athlete in a specialised chamber that is sealed around the waist, and the chamber is then pressurised with air. The LBPP therapy reduces the effective weight-bearing load on the lower extremities, allowing individuals to engage in activities with less impact on their joints and muscles.
Return to sport protocol for calf strains
A return to play strategy is crucial for athletes recovering from muscle strain, especially from lower limb muscle strains. Such a strategy is essential to ensure that the athlete can safely return to their sport without further injury or re-injury. It also helps to gradually reintroduce the athlete to physical activity, allowing them to regain strength, endurance and neuromuscular control while minimising the risk of setbacks. Therefore, physiotherapists must carefully design and implement a return to play strategy for athletes.
Here are a few calf strain specific test to do before starting to run:
- Standing single leg heel raise 25-30 reps full ROM | NO PAIN
- Single leg hopping in place 12-20 reps | NO PAIN
When designing a programme here is 6 recommendations:
- Running should be done on alternative days to start
- Avoid prescribing prolonged, slow continuous running – especially if soleus strain
- Do not progress volume & intensity on consecutive days – give the tissues time to adjust & recover
- Run before calf exercises (if doing it on the same day)
- Running should meet the demands of your sport – Don’t run more than you need to.
- Avoid sudden changes of surface/footwear
Guidelines
Guidelines are from NICE and this is a summarised version for your convenience. Visit for a more robust information. These guidelines are for muscle, tendon & ligament sprains and strain, and not calf strain specifically.
Management of suspected sprain or strain in primary care:
Referral to an emergency department if any of the following are present or suspected:
- Fracture or dislocation
- Damage to nerves or circulation
- Wound penetrating the joint or known bleeding disorder
- Serious complication such as hemarthrosis or septic arthritis
- Full tendon rupture
- Complete tear or tear of more than half the muscle belly
- Large intramuscular haematoma
Advise on the use of analgesia for symptom relief including cautions and contraindications.
Advise on initial ‘PRICE’ self-management strategies for the first 48-72 hours after injury. Protection
Rest
Ice
Compression
Elevation
- Advise on safe return to usual activities and sports and sources of information and support.
- Consider arranging medical review after 5-7 days if there is lack of expected improvement or worsening symptoms.
- Consider arranging a routine referral to physiotherapy if the person has ongoing symptoms.
Advise on preventing re-injury:
- Develop a balanced fitness programme that incorporates cardiovascular exercise, strength training, and flexibility
Avoid exercising or playing sport when tired or in pain Schedule regular days off from exercise Manage any factors that increase the risk of re-injury or falls, where possible
Other conditions you should be aware off
When diagnosing a calf strain, clinicians should also be aware of other conditions that can cause similar symptoms, such as:
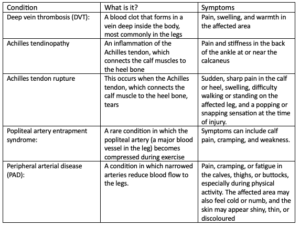
Compared to a calf muscle strain, these conditions may have different signs and symptoms, and may require different diagnostic tests to confirm the diagnosis. For example, DVT may be diagnosed with an ultrasound, while Achilles tendon rupture may require a physical examination or imaging test such as an MRI.
Article summary
- Assessment and treatment of muscle injury, particularly calf complex injury, is an essential part of physiotherapy.
- After the subjective assessment, which determines the extent of the injury, the objective assessment includes palpation, which helps identify any tender spots indicating muscle damage, active and passive range of motion testing to evaluate the extent of the injury, and strength testing to assess the ability of the muscle to generate force.
- In the acute phase, treatment involves limiting activities, managing pain, and preventing complications such as haemorrhage, using high compression bandages, and avoiding massage and heat.
- In the subacute phase, the goal is to improve mobility, prevent muscle atrophy or contracture, and facilitate tissue regeneration to optimize functional recovery.
- A structured exercise program, based on the principles of progressive overload, specificity, and individualization, can help patients to safely and effectively recover from their calf strain and improve overall muscle function.
- Examples of exercises are double leg standing heel raises, double leg standing knee bent heel raises, horizontal and lateral heel raises, single leg RDL, and squats.
- Blood flow restriction training is a form of light resistance training that can be beneficial in a clinical and elite sport setting.
Source
- Baoge, L., Van Den Steen, E.L.K.E., Rimbaut, S., Philips, N., Witvrouw, E., Almqvist, K.F., Vanderstraeten, G. and Vanden Bossche, L.C., 2012. Treatment of skeletal muscle injury: a review. International Scholarly Research Notices, 2012.
- Green, B. and Pizzari, T., 2017. Calf muscle strain injuries in sport: a systematic review of risk factors for injury. British journal of sports medicine, 51(16), pp.1189-1194.
- Green, B., McClelland, J.A., Semciw, A.I., Schache, A.G., McCall, A. and Pizzari, T., 2022. The Assessment, Management and Prevention of Calf Muscle Strain Injuries: A Qualitative Study of the Practices and Perspectives of 20 Expert Sports Clinicians. Sports medicine-open, 8(1), pp.1-28.






Leave a Reply