
Frozen Shoulder: Assessing & Managing
As a clinician, encountering perplexing cases of persistent shoulder pain is not uncommon. Enter the world of frozen shoulder—a condition that often disguises itself with early-stage similarities to other shoulder conditions. Recognize the nuances: a gradual surge in pain, diminishing range of motion, and a persistent, nagging ache.
In this article we dive into the assessment, treatment as well as other conditions you should be mindful off.
Enjoy!
Learn about the cause, risk factors and clinical course in our other article – Cracking the code of frozen shoulder: What you need to know
5 Key takeaways of the article
- Diagnosing frozen shoulder can be challenging due to its resemblance to other shoulder injuries, but key signs include gradual pain increase, loss of range of motion, and persistent dull ache.
- Patient history should consider risk factors like trauma, arthritis, diabetes, thyroid issues, and previous shoulder pain.
- Objective assessment involves noting reduced passive range of motion, such as more than 50% loss in external rotation and more than 25% loss in flexion/abduction, compared to the unaffected arm.
- Conservative management encompasses physiotherapy, NSAIDs, and corticosteroid injections, while combining treatments can aid in pain relief.
- Corticosteroid injections are effective in suppressing inflammation and alleviating symptoms during early stages of frozen shoulder but don’t reverse later fibrotic changes.
Assessment – Identifying Frozen Shoulder
Frozen shoulder is relatively simple to diagnose at later stages of the condition, however it can masquerade as all types of shoulder injury in the early stages. To raise your suspicions from a subjective point of view you want to listen out for:
- Gradual increase in pain
- Gradual loss of range of motion
- Dull ache throughout the day
You would want to find out if the patients has risk factors associated with frozen shoulder
And whilst it wont help to diagnose, gather if the patient has
- Had a traumatic event (fracture, fall, dislocation)
- Arthritis
- Diabetes
- Thyroid issues
- Previous history of shoulder pain
This will help to piece the information, and if enough flags are noticed, it will help lead the clinical management.
To increase the suspicion of frozen shoulder even further, the following needs to be observed in the
Objective assessment
- Reduced passive range of motion of >50% in external rotation (compared to opposite arm)
- Reduced passive range of motion of >25% in flexion and abduction (compared to opposite arm)
Early management
Initial Approach and Conservative Management:
Conservative methods are preferred for treating adhesive capsulitis, especially before considering surgery. Surgery is considered for cases where non-invasive treatments are unsuccessful.
Early Combined Treatment Approach:
In the beginning stages, a combination of physiotherapy, NSAIDs (anti-inflammatory medication), and corticosteroid injections into the joint can be effective. This approach is beneficial when pain is a significant symptom.
First-Line Options and Uncertain Benefits:
Both NSAIDs and physiotherapy have historically been commonly used for treating early adhesive capsulitis. However, it’s not definitively proven that either treatment alone provides clear therapeutic benefits.
Limitations of Physiotherapy in Later Stages:
Physiotherapy is generally not recommended beyond the initial stages of the condition. It might have limitations in addressing the advanced stages of adhesive capsulitis.
Key Treatment Modalities:
The primary treatment methods used for frozen shoulder are physiotherapy and corticosteroid injections.
Effectiveness of Corticosteroid Injections:
There is reasonable evidence supporting the use of corticosteroid injections directly into the joint for treating frozen shoulder.
Corticosteroid Impact on Inflammation and Fibroblasts:
Corticosteroids have a broad suppressive effect on inflammation in the joint. They also hinder the transformation of fibroblasts into myofibroblasts, which contribute to tissue stiffness.
Timing of Corticosteroid Injection:
Administering corticosteroid injections early in the disease process has a greater impact on reducing clinical symptoms.
Limitations of Corticosteroids:
While corticosteroids can suppress inflammation, they cannot reverse later fibrotic changes that occur in the progression of the condition.
Mechano-sensitivity and Pain Threshold:
Physiotherapy techniques that exceed the pain threshold early in the disease process can have negative effects. Fibroblasts, which are sensitive to mechanical stress, might be influenced by the ongoing inflammatory response

Other treatments to consider
More invasive treatments are considered when conservative approaches haven’t been effective for 2-3 months. Some experts propose trying non-surgical methods for up to 6 months before considering invasive options.
One of those treatments is manipulation under anaesthesia is a procedure where the joint is manipulated while the patient is under pain relief. It is well-tolerated and can lead to improved range of motion (ROM) within a few days. However, this may not be long term
Other treatments consist of:
NSAIDs for Pain Relief:
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) can provide short-term pain relief in early stages of the condition. They work by suppressing the activity of COX-1 and COX-2 enzymes, which are involved in synovitis-related inflammation.
Hypertonic Saline Administration:
Hypertonic saline, when administered, may be more effective than normal saline. Intra-Articular
Hydraulic Distension:
This technique involves injecting fluid into the joint to improve pain and function in the short term. Benefits are noticeable up to 3 months after the procedure. Diabetic patients might have less favourable outcomes compared to non-diabetic patients.
Stretching Exercises for Collagen Remodelling:
Controlled stretching exercises, up to a tolerable level of pain. The gentle tensile pressure can favours collagen remodelling, which is important for tissue healing. A study by Lubis and colleagues found that stretching exercises were superior to supervised neglect.
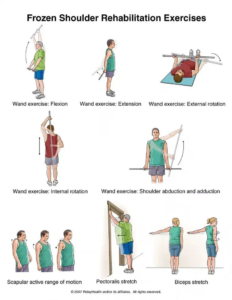
Exercise based management
Whilst the evidence shows that exercise does not improve range of motion or decrease symptoms and progression of the condition, its still recommended for patients to participate in exercise that does not cause them discomfort to help with pain tolerance, internal locus of control and overall well being,
For frozen shoulder we typically focus on two areas:
- Thoracic ROM2
- Rotator cuff activation
Depended on shoulder irritability during movements here are a few exercises that can be prescribed
High irritability
- Using stick for assistance – External rotation (2 sets-10/15 reps) | 1-2x a day
- Supine flexion with stick (2 sets -10/15 reps) | 1-2x a day
- Thoracic mobility | Rotation & extension (2 sets-10/15 reps) 1-2x a day
- Isometric Internal/external rotation (at door frame) and abduction (3 sets /30sec)
Moderate irritability
- Active external rotation (start at elbows to the side and move to 90 degrees as pain allows)
- Supine flexion with weighted stick (2 sets-10/15 reps) | 1-2x a day
- Thoracic mobility | Rotation & extension (2 sets-10/15 reps) | 1-2x a day (Rotation: hand wide and reaching as far as possible | Extension: Arms behind shoulder)
- Banded internal/ external rotation & lateral raise (90degrees) (3 sets – 10-15 reps) 2-3x a week
Low irritability
- Can do same us moderate irritability or progress further if appropriate (as pain allows)
- Weighted supine external rotation
- Weighted supine single arm pullover (4 sets – 10-15 reps) 2-3x a week
- Thoracic rotation (Follow hand with eyes through a full up and down rotation of hand)
Guidelines From NICE
The following is the summarised guidelines from NICE, for your convenience:
Visit the website for a more comprehensive overview
Diagnosis and Expectations:
- Pain and stiffness are main symptoms.
- Pain is worse initially, especially at night.
- Pain improves gradually, but stiffness worsens and then resolves.
- Condition is self-limiting but can take months to years to resolve.
Activity Modification and Pain Control:
- Use arm for movement but avoid painful movements.
- Consider time off work or leisure activities.
- Use analgesia as advised.
- Hot packs may help.
- Support arm with pillows in bed.
Management Considerations:
- Start with non-invasive treatments.
- Consider severity of symptoms and impact on daily life.
- Offer analgesia, especially in early phase.
- Consider paracetamol first, then NSAIDs or codeine.
- Consider physiotherapy: 6-week course, can be extended if improving.
- Physiotherapy includes education, exercises, manual therapy, etc.
- Intra-articular corticosteroid injection if no progress with conservative treatment. Injection can be done by appropriately trained person. Monitor for potential adverse effects, especially in diabetes.
Other Conditions You Should Be Aware Of
| Condition | Symptoms |
| Rotator Cuff Tears: | Similar to tendinopathy but may include more significant weakness, sudden pain if tear is traumatic, limited range of motion, clicking or popping sounds during movement. |
| Rotator cuff related shoulder pain | Persistent deep shoulder pain, weakness when lifting or moving the arm, limited range of motion, discomfort at night, and cracking sensations. Usually discomfort gets worse with activity and overhead shoulder movements. |
| Labral Tears (SLAP Tears): | Deep, dull shoulder pain, clicking or popping with movement, feeling of instability, pain with lifting or carrying objects |
| Biceps Tendinopathy: | Frontal shoulder pain, worsens with overhead activities or lifting, pain radiating down the upper arm, tenderness in the front of the shoulder. |
| AC Joint Sprain or Arthritis: | Localized pain and tenderness over the AC joint at the top of the shoulder, pain worsens when crossing arms or lifting objects. Glenohumeral (Shoulder) |
| Arthritis | Gradual onset of shoulder pain and stiffness, limited range of motion, pain worsens with movement and weight-bearing |
| Thoracic Outlet Syndrome: | Numbness or tingling in the arm or fingers, pain in the neck, shoulder, and arm, weakness in the hand, worsens with certain arm positions |
| Nerve Entrapment (e.g., Suprascapular Nerve): | Deep ache or burning pain in the shoulder, weakness in specific movements, discomfort may radiate down the arm. Referred Pain (e.g., Cervical Radiculopathy): Symptoms: Neck pain with radiation into the shoulder, arm, or fingers, tingling or numbness along the arm or hand |
| Fractures or Dislocations: | Sudden, severe pain after trauma, visible deformity, limited range of motion, possible swelling or bruising |
Summary Of Article
- Diagnosing early-stage frozen shoulder is tricky; watch for gradual pain, range loss, and dull ache.
- Consider risk factors, trauma, arthritis, diabetes, thyroid, prior shoulder pain. Objectively, check reduced passive motion: >50% external rotation, >25% flexion/abduction.
- Conservative management: physio, NSAIDs, corticosteroids; early combined treatment for pain.
- Corticosteroid injections help early inflammation but not late fibrosis; invasive options if conservative fails.
- Other treatments: NSAIDs, hypertonic saline, hydraulic distension, controlled stretches.
- Exercise advised for pain tolerance and well-being, not ROM improvement.
- NICE guidelines highlight pain, stiffness, suggest activity modification, pain control, physiotherapy, corticosteroid injections.
Sources
- Hand, C., Clipsham, K., Rees, J.L. and Carr, A.J., 2008. Long-term outcome of frozen shoulder. Journal of shoulder and elbow surgery, 17(2), pp.231-236
- Kraal, T., Lübbers, J., van den Bekerom, M.P.J., Alessie, J., van Kooyk, Y., Eygendaal, D. and Koorevaar, R.C.T., 2020. The puzzling pathophysiology of frozen shoulders–a scoping review. Journal of Experimental Orthopaedics, 7(1), pp.1-15.
- Lubis, A.M.T. and Lubis, V.K., 2013. Matrix metalloproteinase, tissue inhibitor of metalloproteinase and transforming growth factor-beta 1 in frozen shoulder, and their changes as response to intensive stretching and supervised neglect exercise. Journal of Orthopaedic Science, 18, pp.519-527.






Leave a Reply