
Achilles Tendinopathy: Assessment & Treatment
Are you struggling with Achilles tendinopathy and looking for effective solutions? Look no further! Welcome to our article, where we’ll guide you through the essential aspects of this condition, including assessment, return to sport, acute management, and exercise-based management.
Whether you’re a young professional or a clinical veteran, we’ve got you covered. Join us as we dive into the world of Achilles tendinopathy and explore proven strategies to help you treat your patients.
Get ready to discover the path to recovery and get your clients back in the game!
To learn about risk factors and clinical presentation click here
5 key takeaways
- Assess Achilles injuries through visual observation, gentle touch, and movement evaluation
- Use tests like the squeeze test and palpation to assess the tendon’s condition & rule out rupture
- Manage acute pain using a pain rating scale and avoid increasing pain or stiffness week by week
- Exercise-based treatments, especially eccentric exercises, improve tendon function and reduce pain
- Consider alternative treatments if exercise therapy doesn’t work, such as orthoses or shockwave therapy
Assessment – Look, Feel, Move Principle
The “Look, feel, move” principle is a useful and simple approach used to help gather more information about an injury before moving on to more specific tests. This principle can help you assess and diagnose injuries more effectively.
-
- Start by looking at the injury. Observe the affected area for any visible signs like swelling, bruising, or deformities. As well as color, shape, and symmetry compared to an un-affected ankle. This visual inspection provides important clues about the nature and severity of the injury.
- Move on to feeling the injury. Use your hands to gently touch and feel the ankle joint. Pay attention to any tenderness, swelling, or unusual sensations. This step helps you gather more information about the injury and determine specific points of concern.
- Assess the movement of the injured body part. Ask the patient to actively move the area if possible, then passively check the range. Observe for any pain, limitations, or abnormal movements during this process.
Special tests
We went over the basic assessment that can be used to assess any joint. Now, lets have a look at more achilles tendon specific assessments:
Squeeze test:
If a patient comes walking in then this test is un-necessary as it means the achilles is intact, however if patient comes in with crutches or if you’re in an acute situation (sports games/training) it’s an important test to do.
Squeeze test is an easy test that allows us to determine if the Achilles tendon is fully ruptured.
To perform follow a 3-step process:
-
- Ask the patient to lie face down or sit with their legs hanging off the edge of an examination table, ensuring their feet are relaxed and not actively contracted.
- Gently squeeze the calf muscles just above the heel using your hands or thumbs. Apply moderate pressure and assess the patient’s response. A positive test is indicated by pain or discomfort in the area of the Achilles tendon, which may suggest a potential injury or inflammation.
- Compare the results with the opposite side for a baseline comparison and document your findings accordingly.
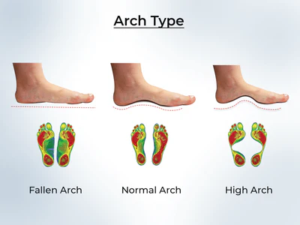
Foot arches and ROM:
Inspect the foot and heel for malalignment, which can have implications for biomechanics and be potential cause of injury. Look for excessive foot pronation, where the arch collapses and the foot rolls inward excessively and for forefoot varus, a position where the front of the foot tilts inward. These can lead to imbalance and stress on the foot and ankle. Additionally, reduced ankle dorsiflexion can affect gait and increase load on the tendon.
Palpation:
The Tendon should be palpated for localised thickening, nodularity, tenderness, and crepitus. Note the findings and compare them in the follow-up to determine positive/negative changes. Let the results guide your treatment.
Calf endurance:
For the Achilles tendon the muscular endurance of the calf complex unit is assessed by the calf-raise or toe-raise test.
To perform the test follow 6 steps
-
- Have the patient perform single-legged heel rises on a 10° incline with their habitual shoes and fingertip support on a wall for balance.
- Heel-rise cycle cadence should be set at 60 per minute using a metronome.
- Instruct to lift the heel as high as possible, maintaining straight knee and trunk position.
- Verbal feedback can be provided to maintain test parameters and encourage continued performance until exhaustion.
- Terminate the test if subjects can’t lift the heel, maintain pace, knee angle, trunk position, or rely on fingertip support or wall assistance.
- The number of correct heel rises completed for each leg is recorded as the outcome score, with one verbal reminder allowed before test termination
We are expecting to see 25+ repetitions, if the number is lower that means calf complex endurance is not at an optimal level.
Look for deference between the two sides as well, if the left can do 34 and the right 24 that means that it may be a good option to address the discrepancy
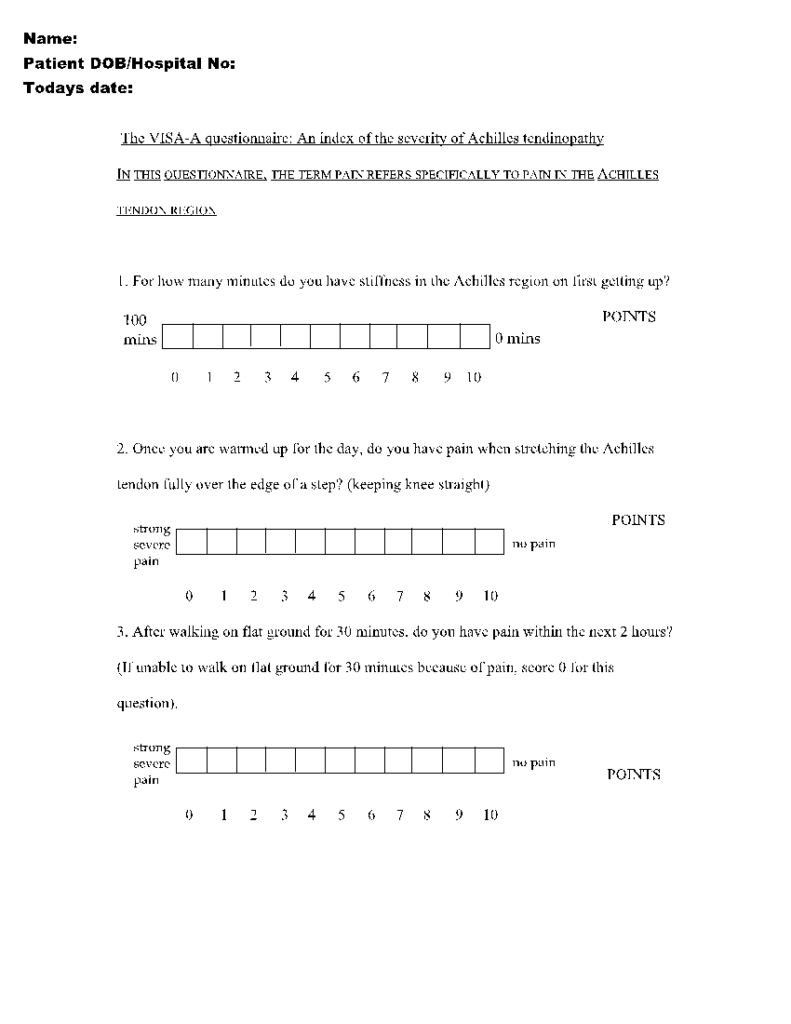
Subjective outcome measures –
VISA-A for Achilles questionnaire to assess pain & dysfunction is a perfect way to test recovery subjectively and determine if the treatment plan is working. You can perform this test every 3-4 weeks and can be done before consultation to save face-to-face time.
 Early Management of Achilles Tendinopathy
Early Management of Achilles Tendinopathy
Acute management of Achilles tendinopathy is determined by the pain that the patient experiences during single leg raise from a 25 degree declined wedge or a elevated surface (dependent If the tendinopathy is insertional on non-insertional). Good way to gage pain is to us Numerical Pain Rating Scale (NPRS). The following guidelines are set out by Silbernagel and coleagues
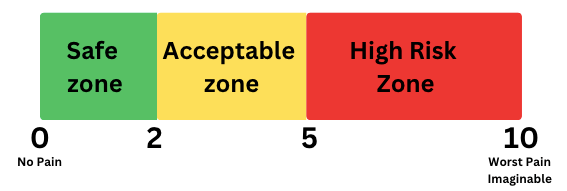 4 points of principle:
4 points of principle:
-
- The pain is allowed to reach 5 on the NPRS during activity
- The pain after activity is allowed to reach 5 on the NPRS
- The pain morning after the exercises should not be higher than 5
- Pain and stiffness should not increase from week to week
Eccentric exercises have been found to be both safe and highly recommended in the acute treatment of Achilles tendinopathy. Research suggests that these exercises can effectively alleviate symptoms and promote tendon healing without causing harm. They involve controlled lengthening of the tendon, which helps to improve tendon strength, reduce pain, and enhance functional recovery.
Here is the proposed eccentric exercise protocol from Silbernagel and colleagues
| Exercise | Dosage | Progression |
| Heel drop knee straight :Stand on the edge of a step on the involved side. Start with standing on the toes, then lower the heel as far down as possible. Rise back on the toes with the assistance of the other foot | 3 sets of 15 reps2x a day
7 days a week for 12 weeks |
Do exercise even if painful (stop if pain is above 5 or is worsening next day) & perform until becomes pain freeOnce pain free progressively add loads in either a backpack or hand until exercise is pain free again |
| Heel drop: Knee bentSame as above but keep the knee of the involved side slightly bent | 3 sets of 15 reps2x a day
7 days a week for 12 weeks |
***Patient dependent, gage motivation level and only prescribe the amount you know they will do***
The best plan is the one that is adhered to
Exercise-based management
Exercise-based treatment for Achilles tendinopathy has shown significant benefits in promoting healing, reducing pain, and improving function.
Here are some reasons why exercise-based treatment is beneficial, supported by evidence:
1. Tendon Adaptation:
Exercise stimulates tendon adaptation and remodelling, leading to improved tendon structure and function. Eccentric exercises, in particular, have been shown to induce positive changes in tendon composition and mechanical properties. A systematic review by Woodley et al. (2007) found that eccentric exercise interventions were effective in reducing pain and improving function in patients with Achilles tendinopathy.
2. Load Management:
Exercise-based treatments allow for controlled loading of the Achilles tendon, which is crucial for tendon healing and recovery. Tendons respond positively to appropriate mechanical loading by increasing collagen synthesis and promoting tendon tissue remodelling. A study by Silbernagel et al. (2007) demonstrated that a progressive tendon-loading program led to significant improvements in pain and function in patients with Achilles tendinopathy.
3. Strengthening and Conditioning:
Specific exercises targeting the calf muscles, such as calf raises and eccentric exercises, help strengthen and condition the muscles and tendons involved in Achilles function. Strengthening these muscles can offload stress from the tendon, enhance shock absorption, and improve overall lower limb biomechanics. A randomized controlled trial by Mafi et al. (2018) showed that a 12-week exercise program focusing on eccentric training led to significant improvements in pain, function, and tendon structure in patients with mid-portion Achilles tendinopathy.
4. Pain Reduction and Function Improvement:
Exercise-based treatments have been shown to effectively reduce pain and improve functional outcomes in individuals with Achilles tendinopathy. A systematic review and meta-analysis by Irby et al. (2020) concluded that exercise interventions, particularly eccentric exercises, were superior to other treatments in reducing pain and improving function in patients with Achilles tendinopathy.
5. Long-Term Benefits:
Exercise-based treatments for Achilles tendinopathy have been associated with long-term benefits and reduced recurrence rates. A study by Vand der Plas (2012) demonstrated that a 12-week eccentric training program resulted in sustained improvements in pain and function, with low recurrence rates at a long-term follow-up of 5 years.
Exercise Based Management Ideas
Non insertional calf raise progression:
- Double leg STANDING elevated (3 sets15 reps)
- Single leg elevated (3 sets15 reps)
- Single leg elevated with weight (3 sets8-12 reps))
Insertional calf raise progression:
- Double leg STANDING heel raises (3 sets25 reps)
- Single leg (3 sets15 reps)
- Single leg with weight (3 sets8-12 reps)
Complimentary Exercises:
- Tibialis anterior curls
- Squat
- Inversion/Eversion of ankle
- Hamstring Bridge
- Single leg squat/Bulgarian squat
- Single leg Balance
Other Types Of Treatment
It is recommended to initially treat all patients with exercise therapy for at least 3 months prior to considering other treatment options. If exercise-based protocol does not help then the following treatment options can be considered.
- Foot orthoses
- Electrical stimulation
- Injection therapies (using platelet-rich plasma, autologous blood, corticosteroids, high- volume saline, sclerosing agents, protease inhibitors, and hyperosmolar dextrose)
- Shockwave therapy
- Low-level laser therapy

Return To Sport
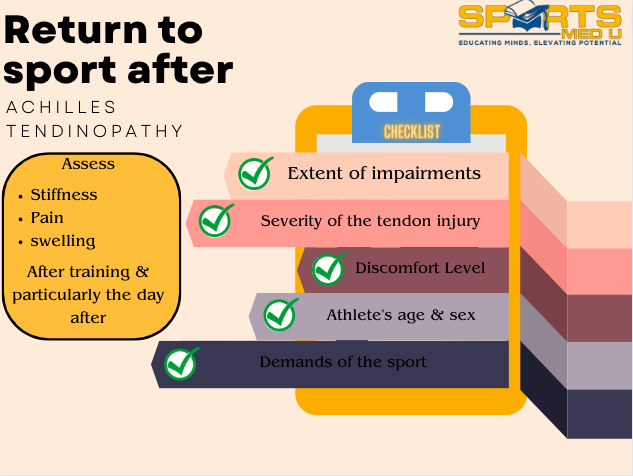
When planning for return to sport programme, several factors need to be taken into account, including the severity of the tendon injury, the athlete’s age and sex, the level of pain and symptoms, the extent of impairments, and the demands of the sport.
During the return-to-sport phase, it is crucial to follow a gradual and controlled progression that allows sufficient time for the athlete to recover and enables the therapist to evaluate symptoms effectively.
Assessing symptoms such as stiffness, pain, and swelling after training, particularly the day after, can help determine appropriate increases in training intensity or volume.
Generally, resuming activities like running and jumping is recommended when the symptoms have subsided. Evidence suggests that sport-related activity does not have a detrimental impact on recovery. However, striking a balance between a swift return to full activity and preventing overloading and re-injury of the tendon is essential during the return-to-sport phase.
NICE Guidelines
Guidelines are from NICE and this is a summarised version for your convenience. Visit NICE for a more robust information.
- Tendinopathy is a condition characterized by pain, swelling, and impaired function of a tendon.
- The Achilles tendon, made up of fibres from the gastrocnemius and soleus muscles, is the thickest and strongest tendon in the body and commonly affected in active people.
- Complications of Achilles tendon injury include tendon rupture, negative impact on daily activities and work, and limitation in sports.
- Symptoms of Achilles tendinopathy include aching (occasionally sharp) pain in the heel, stiffness in the tendon, tenderness, swelling, and crepitus along the tendon.
- Management in primary care includes identifying and managing underlying causes, using cold packs or ice after acute injury, simple analgesia for pain relief, advice on rest, and referral to physiotherapy if symptoms persist.
- Referral to a sports physician or orthopedics is recommended for patients with chronic Achilles tendinopathy or those who fail to respond to conservative treatments.
- Same-day assessment by an orthopedic specialist is required if Achilles tendon rupture is suspected.
Other Conditions To Be Aware Off
True tendon pain (from rupture or tendinopathy) is usually confined to the tendon itself. Other diagnoses that cause pain in and around the Achilles tendon include:
| Condition | Characteristics & symptoms |
| Retrocalcaneal bursitis | A condition characterized by inflammation of the bursa located between the Achilles tendon and the heel bone (calcaneus). The bursa is a small fluid-filled sac that acts as a cushion and reduces friction between the tendon and the bone. Retrocalcaneal bursitis typically occurs due to repetitive friction or pressure on the area, leading to pain, swelling, and tenderness at the back of the heel. It is commonly seen in activities involving repetitive ankle movements, such as running, jumping, or wearing ill-fitting shoes |
| Dislocation of the peroneal or other plantar flexor | Dislocation of the peroneal tendons is a relatively uncommon but painful injury that occurs when one or both of the peroneal tendons in the foot slip out of place from their normal position behind the lateral malleolus (the bony protrusion on the outside of the ankle). The peroneal tendons are responsible for the outward movement of the foot and ankle, and they can be subjected to stress and trauma during sports or other physical activities. Symptoms of peroneal tendon dislocation may include pain, swelling, and instability in the ankle joint, as well as difficulty walking or standing |
| Posterior ankle impingement | Posterior ankle impingement is a condition that occurs when there is compression or pinching of soft tissues (such as tendons, ligaments, or nerves) in the back of the ankle joint. It is often caused by repetitive or excessive movements that lead to inflammation and swelling of the soft tissues. This can result in pain, limited mobility, and reduced function of the ankle joint |
| Haglund’s deformity | Haglund’s deformity is a condition characterized by a bony enlargement or protrusion on the back of the heel bone, which can cause pain and discomfort in the affected area. It is also known as “pump bump” because it is often associated with wearing tight-fitting shoes, such as high heels or pumps, that rub against the back of the heel bone. The bony enlargement can also cause irritation and inflammation of the Achilles tendon, which attaches to the back of the heel bone. Symptoms of Haglund’s deformity may include pain, swelling, redness, and stiffness in the heel area, as well as difficulty wearing shoes |
| Ostrigonum syndrome | Ostrigonum syndrome is a condition that occurs when the ostrigonum, a small extra bone at the back of the ankle, becomes irritated or inflamed. This extra bone can form during childhood development, and may not cause any symptoms until later in life when it is subjected to repetitive or excessive movements, such as during sports or physical activity. Symptoms of Ostrigonum syndrome may include pain, swelling, and tenderness at the back of the ankle, as well as difficulty moving the ankle joint. The condition is more common in athletes who participate in activities that involve repetitive ankle plantar flexion, such as ballet dancing, soccer, and gymnastic |
| Calcaneal fracture | A calcaneal fracture is a type of bone fracture that occurs in the heel bone (calcaneus), which is one of the largest bones in the foot. The injury can result from a sudden impact, such as a fall from a height, a car accident, or a sports-related injury. Calcaneal fractures can range from mild to severe, and may be classified based on the number and location of the fracture lines. Symptoms of a calcaneal fracture may include pain, swelling, tenderness, and difficulty walking or bearing weight on the affected foot. In some cases, the skin over the affected area may be visibly bruised or damaged. Treatment options for calcaneal fractures may include rest, immobilization with a cast or brace, pain management, physical therapy, and in some cases, surgery |
| Irritation or neuroma of the sural nerve | Irritation or neuroma of the sural nerve is a condition in which the sural nerve, a sensory nerve that runs along the back of the lower leg and foot, becomes inflamed, irritated or compressed, resulting in pain, numbness, tingling or burning sensations. This condition may occur due to various factors such as injury, trauma, overuse, or abnormal anatomy. Symptoms of sural nerve irritation or neuroma may include pain, numbness, or tingling sensations in the back of the foot and ankle, which may radiate upwards along the leg. The condition can be diagnosed through a physical examination and may require imaging studies, such as an ultrasound or MRI, to confirm the diagnosis. Treatment options may include rest, ice, anti-inflammatory medications, physical therapy, or injection of a local anesthetic or corticosteroid into the affected area. In |
Summary of article
Assessment:
- Look: Observe the injury for visible signs like swelling, bruising, and deformities.
- Feel: Gently touch and feel the ankle joint to assess tenderness, swelling, and unusual sensations.
- Move: Evaluate the movement of the injured area by asking the patient to actively and passively move it, looking for pain, limitations, or abnormal movements.
Special tests:
- Squeeze test: Squeeze the calf muscles just above the heel to check for pain or discomfort, indicating a potential Achilles tendon injury or inflammation.
- Foot arches and ROM: Inspect the foot and heel for malalignment, excessive pronation, and reduced ankle dorsiflexion, which can affect biomechanics and increase tendon load.
- Palpation: Palpate the tendon for thickening, nodularity, tenderness, and crepitus, comparing findings for changes over time.
- Calf endurance: Assess calf muscle strength with the calf-raise or toe raise test, recording the number of correct heel rises completed.
Acute management:
- Use the Numerical Pain Rating Scale (NPRS) during single-leg raise to gauge pain. Guidelines by Silbernagel et al.:
- Allow pain up to 5 on the NPRS during activity and after activity, with the morning-after pain not exceeding 5.
- Pain and stiffness should not increase from week to week.
Exercise-based management:
- Exercise stimulates tendon adaptation and remodelling, improving tendon structure and function.
- Controlled loading through exercises promotes tendon healing and recovery.
- Specific exercises strengthen calf muscles, offload stress from the tendon, and improve biomechanics.
- Exercise interventions, especially eccentric exercises, reduce pain and improve function in Achilles tendinopathy patients.
- Exercise-based treatments have long-term benefits and low recurrence rates.
Other treatment options:
- If exercise therapy doesn’t help, consider foot orthoses, electrical stimulation, injection therapies, shockwave therapy, or low-level laser therapy.
Return to sport (RTS):
- Consider the severity of the tendon injury, athlete’s age and sex, pain level, impairments, and sport demands when planning RTS.
- Gradual and controlled progression is crucial for athlete recovery and symptom evaluation.
- Assess symptoms after training to determine appropriate training intensity or volume increases.
- Resuming running and jumping is generally recommended when symptoms subside.
- Balancing a swift return to activity with avoiding overloading and re-injury is important during RTS.
Sources
- Grävare Silbernagel, K. and Crossley, K.M., 2015. A proposed return-to-sport program for patients with midportion Achilles tendinopathy: rationale and implementation. journal of orthopaedic & sports physical therapy, 45(11), pp.876-886.
- Hébert-Losier, K., Wessman, C., Alricsson, M. and Svantesson, U., 2017. Updated reliability and normative values for the standing heel-rise test in healthy adults. Physiotherapy, 103(4), pp.446-452.
- Irby, A., Gutierrez, J., Chamberlin, C., Thomas, S.J. and Rosen, A.B., 2020. Clinical management of tendinopathy: a systematic review of systematic reviews evaluating the effectiveness of tendinopathy treatments. Scandinavian journal of medicine & science in sports, 30(10), pp.1810-1826.
- Mafi, N., Lorentzon, R. and Alfredson, H., 2001. Superior short-term results with eccentric calf muscle training compared to concentric training in a randomized prospective multicenter study on patients with chronic Achilles tendinosis. Knee Surgery, Sports Traumatology, Arthroscopy, 9, pp.42-47.
- Paavola, M., Kannus, P., Järvinen, T.A., Khan, K., Józsa, L. and Järvinen, M., 2002. Achilles tendinopathy. JBJS, 84(11), pp.2062-2076.
- Suan Cheng Tan & Otto Chan (2008) Achilles and patellar tendinopathy: Current understanding of pathophysiology and management, Disability and Rehabilitation, 30:20-22, 1608-1615, DOI: 10.1080/09638280701792268
- Van der Plas, A., de Jonge, S., de Vos, R.J., Van Der Heide, H.J.L., Verhaar, J.A.N., Weir, A. and Tol, J.L., 2012. A 5-year follow-up study of Alfredson’s heel-drop exercise programme in chronic midportion Achilles tendinopathy. British journal of sports medicine, 46(3), pp.214-218.
- Woodley, B.L., Newsham-West, R.J. and Baxter, G.D., 2007. Chronic tendinopathy: effectiveness of eccentric exercise. British journal of sports medicine, 41(4), pp.188-198.






Leave a Reply